Recently, I was reading an article discussing the differences in symptoms among adults with canal versus otolith vestibular dysfunction, which raises some important questions for the future of vestibular assessment. As most clinicians know, a detailed case history is essential in establishing a diagnosis of peripheral vestibular dysfunction, with the qualitative nature of the symptoms being important in reaching a final diagnosis.
A traditional symptom of peripheral vestibular system dysfunction is rotary vertigo, meaning a sensation of self or environmental motion. Symptoms are then evaluated with objective measures, such as calorics (horizontal canal) or dynamic positioning tests (typically posterior canal) to reach an end diagnosis.
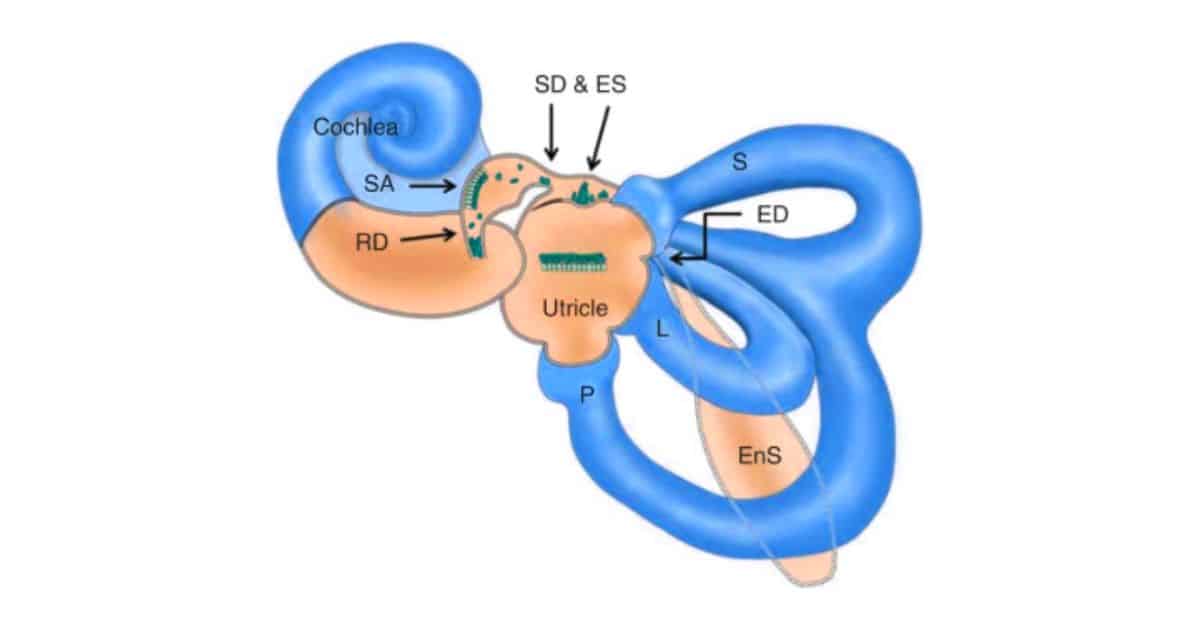
In the past, these objective measures have predominately focused on assessment of semicircular canals (head turn sensors), which have different end functions than the otolith organs (linear sensors) of the vestibular system. Therefore, it seems logical that dysfunction of the semicircular canal(s) of the vestibular system may provoke different symptoms than otolith dysfunction. Otolith dysfunction (saccule and/or utricle) may then produce non-typical symptoms, which may still be indicative of peripheral vestibular system damage such as: tilting, pushing/pulling, or rocking sensations due to their contribution in sensing linear acceleration, postural control, and head tilt.
Objective measures like calorics and dynamic positioning tests have primarily focused on assessing the semicircular canals, which have distinct functions from the otolith organs. Dysfunction in the otolith organs, responsible for sensing linear acceleration, postural control, and head tilt, may result in non-typical symptoms such as tilting, pushing/pulling, or rocking sensations. While assessment of otolith dysfunction through VEMP testing has gained traction in recent years, there is still much to uncover about its effects.
It has only been in recent years that assessment of the otolith organs (saccule & utricle) of the vestibular system have become more widely utilized with VEMP testing, so less is known of the effects of their dysfunction.

Vestibular System Dysfunction: Symptoms & Treatment
In the aforementioned article, the authors were able to assess individuals with varying pathologies and degrees of vestibular system dysfunction. They were able to successfully categorize individuals based off of their symptomology as having semicircular canal versus otolith involvement using a symptom index of their creation. Individuals with semicircular canal pathology tended to have symptoms of rotary vertigo, while those with otolith damage reported more linear symptoms including pulling/pushing, rocking, or tilting sensations.
While all of the individuals were found to be unsteady on their feet, those with otolith organ involvement reported higher handicap due to their symptoms and were at a much higher risk for falling than those with semicircular canal dysfunction only.
There were several limitations to this preliminary report, including the small sample size, but this does call for clinicians working with dizzy patients to be more open-minded in what quantifies a symptom of vestibular dysfunction. Linear symptoms such as pulling/pushing, tilting, or rocking sensations may then be appropriate for clinicians to accept as symptoms of vestibular system dysfunction, with differential evaluation necessary to rule in or out otolith involvement. This report further elucidates the need for comprehensive evaluation of the vestibular system, including both the semicircular canals and otolith organs, in order to appropriately direct therapy and/or further referrals for diagnostic evaluation.
The current treatment for those identified with unilateral vestibular system damage would be physical therapy designed to stimulate the vestibular system as a means to drive central compensation for the injury. This central compensation is a re-calibration of the vestibular system to make sense of the change in input at the level of the brain. Traditional views of vestibular rehabilitation have focused on stimulating the vestibular ocular reflex through head movements. This type of therapy has been shown to be beneficial, especially in cases of semicircular canal damage. However, in cases of otolith dysfunction it seems that physical therapy targeting postural control and orientation of the head and body may also beneficial, as these appear to be the primary functions of the otolith organs. Currently, there is little evidence to support this claim and further research is necessary in order to determine appropriate diagnosis and therapy options for damaged otolith organs.
Reference:
- Lisa Farrell, Rose Marie Rine, “Differences in Symptoms among Adults with Canal versus Otolith Vestibular Dysfunction: A Preliminary Report”, International Scholarly Research Notices, vol. 2014, Article ID 629049, 10 pages, 2014. https://doi.org/10.1155/2014/629049

Brady Workman, AuD, is an audiologist in the Balance Disorders program at Wake Forest Baptist Health Center. He has authored several articles relating to balance and vestibular disorders as a regular contributor and co-editor of the Dizziness Depot at Hearing Health & Technology Matters. Brady received his doctorate of audiology from East Tennessee State University in 2018 and is licensed by the North Carolina Board of Examiners for Speech Language Pathologists and Audiologists and is a fellow of the American Academy of Audiology.







This is a great article and comments by Brady Workman. We have known for a long time that the SSCs are for determining the angular position of the head, and the otoliths for determining the position of the head in relationship to the body/earth (gravity receptors). I have found that HC BPPV patients have worse symptoms than PC or AC BPPV. Likewise, patients with otolith, or combination otolith/SSC dysfunction, have different symptoms than patients with only SSC dysfunction. The article accurately describes those differences, and raises the question of valid and reliable treatment for otolith dysfunction. We always refer them to PT for postural control as well and indicate that the primary dysfunction appears to be otolith. Keep up the interested articles and comments.
How, if in any way, is otolith dysfunction related to or causal for Mal de Debarquement Syndrome? There are a number of practitioners attempting to make this association but it is difficult to find information about.
Thank you.
Mal de Debarquement Syndrome (MdDS) is generally not thought to be related to a specific injury to the ear or the brain and is a diagnosis of exclusion. Diagnosis is typically made based off of close temporal proximity to a situation of sustained physical motion (e.g. a cruise), normal imaging of brain, normal vestibular function tests and symptoms of rocking or swaying for more than one month. MdDS is thought to be a central phenomenon, most commonly caused by sustained motion from a boat or cruise trip. In cases of MdDS the brain has adapted to the continual rocking movement of the boat beneath the individuals feet and when introduced back onto a stable surface (dry land) the brain has difficulty re-adapting. MdDS is thought to be a potential form of motion sickness. Those with otolith dysfunction are likely to also have rocking or tilting sensations, but this is believed to be separate from a diagnosis of MdDS.
According to the MdDS foundation, MdDS is caused by Vestibular Dysfunction more specifically vestibule-ocular reflex malfunction.
Here’s the study they(including Dr Dai) to come to that conclusion:
https://www.frontiersin.org/articles/10.3389/fneur.2017.00175/full
The MdDS treatment for this is a type of VRT to compensate for the malfunction of the Vestibular dysfunction.