Downstream Consequences of Aging is a bi-monthly series written by guest columnist Barbara Weinstein, PhD.
A continuous two-way process, communication involves the exchange of both verbal and non-verbal messages. Essential to communication are:
- the ability of the sender to encode the information,
- the ability of the recipient to hear, understand, and process the information (aka decode), and
- the opportunity for the recipient to confirm or provide feedback confirming that the message has been interpreted correctly.
Miscommunication or lack of clear communication takes place when there is a breakdown in the encoding or decoding process. For example, the sender may underestimate the needs or abilities of the recipient and/or may overestimate their own effectiveness.
Misinterpretations, Misunderstandings, Mishearings
Similarly, the recipient may misinterpret or fail to provide feedback confirming their understanding of the content of the message. Failure to close the loop in the communication chain can be detrimental. This is especially so in the health care setting wherein 40-80% of medical information patients receive tends to be forgotten immediately and nearly half of the information discussed is incorrectly retained (Kessels, 2003).
Rarely mentioned when physicians discuss physician patient communication are the “mishearings” or “misunderstandings “ due to hearing loss. Oliver Sachs, who had a unique fascination with how people heard or saw things, shared some of his mishearings in one of his final opinion pieces appearing in the New York Times (Sachs, 2015). He correctly surmised that people with hearing loss rarely think to question the accuracy of ambiguous sensory data which is why the “teach back” or “show-me” method of closing the loop is so important in health care (Sachs, 2015; Schillinger et al, 2003). Here are a few of the “mishearings” described by Sachs:
- all-or-noneness RATHER THAN oral numbness
- pontillitis RATHER THAN tonsillitis
- a biography of cancer RATHER THAN a biography of Cantor
A way to confirm that the provider has explained to the patient what they need to know in a manner that the patient understands, teach-back has great potential for audiologists as a way to confirm that our patient’s correctly use and understand the communication strategies necessary to self-manage hearing loss.
Why Care about Physician Patient Communication and Hearing Status
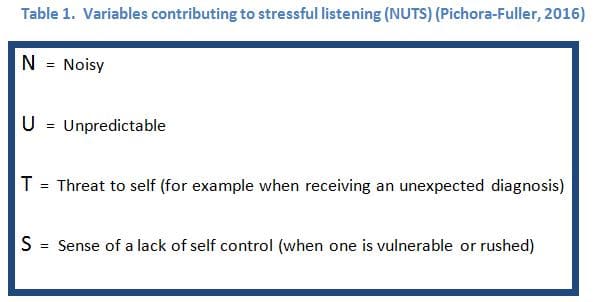
It is probable that stressful listening environments (aka medical encounters) will be associated with “mishearings” especially for vulnerable populations. The sustained listening effort often required when communicating in unfamiliar, noisy and distracting environments may contribute to mental fatigue, thereby impairing decision making (Hornsby & Kipp, 2015; DeLuca, 2005). Pichora-Fuller (2016) provided an apt acronym for stressful listening environments to which we are all exposed (Table 1).
It is in these situations where Hockey’s (2011) motivational control theory of cognitive fatigue comes in to play. Hockey (2011) theorized that fatigue is a protective mechanism humans employ to limit investment of effort in situations the listener concludes h/she has little control. Stated differently, fatigue, reasoned Hockey (2011), is about management of control rather than a lack of energy. Relating this to persons with age related hearing loss (ARHL), the import of our patient’s being counseled about how to self manage their hearing difficulty is magnified.
Effective and efficient communication with patients is essential to knowledge transfer, establishment of caring relationships and quality healthcare (Mick, et al., 2014). Central to building trust, mutual understanding, patient safety and shared decision making, the communication skill set providers bring to the table are key if health needs, expectations and values are to be realized (Spooner et al, 2016). The ability of physicians to gather valid information facilitates diagnosis, the counseling process, health care transitions, and adherence with therapeutic instructions (Ha & Longnecker, 2010). As the ultimate objective of any doctor-patient communication is to improve the patient’s health and medical care, it is not surprising that the two are inextricably intertwined (Ha & Longnecker, 2010).
Recognizing 2-Way Communication Process in Healthcare Settings
It is well established that physicians believe that communication with their patients is paramount. But do they recognize that it is a dynamic, and reciprocal two way process, and that persons with hearing loss have poorer ratings of patient–physician communication and healthcare quality than do persons without hearing loss (Mick et al., 2014)?
ARHL affects 80% of adults over the age of 70 years; the majority of older adults with ARHL do not use hearing aids; and denial of hearing loss is widespread (Chou et al, 2001; Cruickshanks et al, 1998). YET, the culture of health care delivery does not appear to include recognizing or accommodating to the needs of persons with hearing loss. This tendency to overlook hearing status likely has a direct impact on adherence with and recall of physician recommendations.
Borrowing from the Framework for Understanding Effortful Listening (FUEL) espoused by Pichora-Fuller (2016), persons with hearing loss tend to hear with their ears but listen with their brains. Since hearing loss distorts the incoming signal, the hearing impaired must often decide whether it is worth expending the extra cognitive effort necessary to listening and decoding the message from their physician.
For vulnerable populations, when learning of a cancer or dementia diagnosis, the stress associated with such an encounter will likely exacerbate the effort necessary to listen, diverting energy away from cognitive reserves such as memory storage for new information (Pichora-Fuller, 2016). Sadly, the lack of regard for hearing status also appears to be the case in hospice and palliative care settings where communication at this stage of life is highly valued yet increasingly compromised (Smith et al, 2015; Smith et al, 2016).
 What is An Audiologist to Do?
What is An Audiologist to Do?
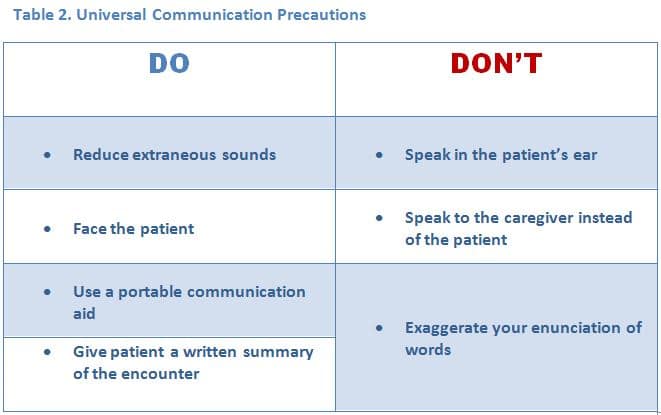
We are all aware of the reasonable assists available for optimizing hearing and communication during routine clinical encounters. Let’s be proactive and develop signage depicting universal communication strategies or precautions physicians should adopt to improve communication with their patients (Table 2).
As part of routine counseling sessions following the audiological evaluation, make sure to encourage your patients to inform their physician/health care provider that they have a hearing loss and how best to communicate with them. It is imperative that you emphasize to your patients that better understanding of their health issues will promote collaborative communication, will enable their physician to be more supportive and will help to optimize adherence to the treatment processes (Ha & Longnecker, 2010).
Also consider demonstrating how to use the various smartphone apps including the Ear Machine or the Jacoti Hearing Suite Listen App. Suggest that your patients who do not own hearing aids invest in the Shure MV88 digital condenser microphone, download the Shure Plus MOTIV app and use it during physician visits. Finally, become part of multi-disciplinary teams working to impose system- level changes in primary care which will help to achieve long-term and sustainable impacts on quality outcomes in clinical practice.
References
Chou R et al. (2011). Screening adults aged 50 years or older for hearing loss: a review of the evidence for the U.S. Preventative Services Task Force. Ann Intern Med. 154: 347e355.
Cruickshanks K et al. (1998) Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin: The epidemiology of hearing loss study. Am J Epidemiol. 148, 879–886.
DeLuca, J. (2005). Fatigue, cognition and mental effort. In J. DeLuca (Ed.), Fatigue as a Window to the Brain (pp. 37-58). Cambridge, MA: MIT Press.
Denes P & Pinson E. (1993). The Speech Chain. 2nd ed. Oxford: WH Freeman and Company.
Ha JF & Longnecker H. (2010). Doctor–patient communication: a review. Ochsner Journal. 10: 38–43.
Hockey, G. R. J. (2011). A motivational control theory of cognitive fatigue. In: P.L. Ackerman (Ed.), Cognitive Fatigue: Multidisciplinary Perspectives on Current Research and Future Applications. (pp 167-187). Washington, DC: American Psychological Association
Hornsby, B. & Kipp, A. (2015). Subjective Ratings of Fatigue and Vigor in Adults with Hearing Loss Are Driven by Perceived Hearing Difficulties Not Degree of Hearing Loss. Ear and Hearing 37: 1-10.
Kessels R. (2003). Patients’ memory for medical information. J R Soc Med. 96:219-22.
Mick P et al. (2014). Hearing loss is associated with poorer ratings of patient-physician communication and healthcare quality. J Am Geriatr Soc. 62:2207–2209.
Pichora-Fuller, K. (2016). How Social Psychological Factors May Modulate Auditory and Cognitive Functioning During Listening. Ear and Hearing. 37: 92S–100S.
Sachs, O. (2015). Mishearings. NYTimes, 6/07/2015.
Schillinger, D., Piette, J., Grumbach, K., et al. (2003). Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 163: 83-90.
Smith, A et al. (2015). Hearing loss in palliative care. J Palliat Med 18:559–562.
Smith, A et al. (2015). Hearing loss in palliative care. J Palliat Med 18:559–562.
Smith A et al (2016). Self-reported hearing in the last two years of life among older adults. J Am Geriatr Soc. 64:1486-1491.
Spooner K et al. (2016). Disparities in perceived patient–provider communication quality in the United States: Trends and correlates. Patient Education and Counseling. 99: 844–854.
First of a Two-Part Series
Barbara E. Weinstein, Ph.D. earned her doctorate from Columbia University, where she continued on as a faculty member and developed the Hearing Handicap Inventory with her mentor, Dr. Ira Ventry. Dr. Weinstein’s research interests range from screening, quantification of psychosocial effects of hearing loss, senile dementia, and patient reported outcomes assessment. Her passion is educating health professionals and the public about the trajectory of untreated age-related hearing loss and the importance of referral and management. The author of both editions of Geriatric Audiology, Dr. Weinstein has written numerous manuscripts and spoken worldwide on hearing loss in the elderly. Dr. Weinstein is the founding Executive Officer of Health Sciences Doctoral Programs at the Graduate Center, CUNY which included doctoral programs in public health, audiology, nursing sciences and physical therapy. She was the first Executive Officer the CUNY AuD program and is a Professor in the Doctor of Audiology program and the Ph.D. program in Speech, Language and Hearing Sciences at the Graduate Center, CUNY.
feature photo courtesy of shannon christy