Hearing difficulty remains one of the most prevalent medical conditions in the United States, according to a recent epidemiological study. Furthermore, and perhaps more troubling to professionals, the majority of individuals with hearing difficulties are not referred to either otolaryngology or audiology for advanced care by their primary care specialist.
Researchers used the National Health Interview Survey (NHIS) to investigate prevalence and other characteristics of self-reported hearing difficulties among adults living in the United States. Unlike similar epidemiological studies, which collect patient data at the point of care, the NHIS gathers representative sample data at the household level. This direct approach to data collection enables researchers to gain an “unfiltered” view of patient attitude and behavior.
Hossein Mahboubi and colleagues from the University of California, Irvine and Harvard Medical School, respectively, gathered and analyzed more than 36,000 surveys on a wide range of demographic, prevalence and other characteristics of self-reported hearing status. No objective information, such as pure tone audiogram thresholds were collected. Despite the lack of objective information, NHIS methodology is considered reliable and valid.
According to the researchers, 40.3 million adults, which equates to 16.8% of the population in the US, had some degree of self-reported hearing difficulty, ranging from “a little trouble with the hearing” to being “deaf.” Further, based on analysis, 21% of the population has problems hearing in background, ranging from “about half the time” to “always.”
A further breakdown of various self-reported hearing characteristics is shown in Table 1, which was taken directly from the JAMA-Otolaryngology report:
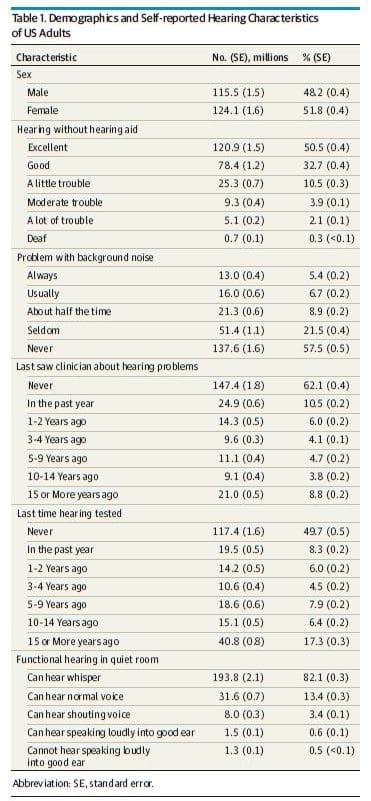
Results of the survey provided several findings: The most common self-reported age of onset of hearing loss was 50-59, followed closely by 40-49 and 60-69. Just over 11% of the population reported that hearing loss caused safety concerns at least “half the time.” Perhaps more problematic, 36% of the population reported they are frustrated with their hearing “about half the time” or more often.
Hearing Loss Flies Under the Radar Too Often
Besides demographic and self-reported hearing loss data, the survey also examined treatment patterns of the adults who reported difficulties with their hearing. It was determined that of the approximately 40.3 million adults with “less-than-good” hearing, 32.2% had never seen a clinician for hearing problems, 48.1% were never referred to a hearing specialist, 45.3% were never referred to an audiologist and 28.0% had never had their hearing tested.
Additionally, hearing aid usage data was collected. This portion of the survey indicated that 7.3 million adults, estimated to be 3.1% of the U.S. population, reported using hearing aids at the time of the survey.
The duration of hearing aid use was broken down into the following three categories based on years of hearing aid use experience: Less than a year for 10.1%, between one and five years for 37.9%, and five years or more in 52.0% of the self-reported hearing aid users. Average hearing aid use per day was also calculated. It was estimated that 63.7% of hearing aid users wore their hearing aids eight hours per day or longer, while 23.0% wore their hearing aids one to seven hours per day and 13.2% wore their devices a one hour per day or less.
Cochlear Implant Candidacy Under Diagnosed and Under Appreciated
The functional capability of individuals with hearing difficulties was focus of the investigators. Of considerable interest, 2.8 million people (1.1% of the population) reported an inability to hear shouting in a quiet room, which is believed to equate to a severe-profound degree of hearing impairment. A mere 5.3% of these adults in this category received a recommendation for a cochlear implant (CI). And of that small percentage referred for a cochlear implant, only 22.1% received a CI.
Despite solid clinical evidence and adequate insurance reimbursement for the CI procedure, the low rate of referral for a CI evaluation in this study is consistent with previous estimates of a 5% utilization rate in the eligible adult population with severe profound hearing loss.
These results suggest an opportunity for otolaryngologists and audiologists to raise awareness among primary care physicians and the general population about the benefits of cochlear implants.
Like other studies, the NHIS data shows a substantial gap between those with self-reported hearing difficulties and hearing aid use. As previously mentioned, just over one-third of the population was reported to have hearing difficulties that caused frustration “at least half the time,” yet 3.1% of the population was estimated to use hearing aids.
In addition, this study shed light on the topic of “hidden hearing loss,” as 50.3 million individuals (21% of the population) reported to have some degree of trouble with hearing in background noise. This is a number far higher than the 40.2 million individuals estimated to have hearing that was “less-than-good.” This gap between self-reported difficulties in noise and self-reported hearing loss might reflect in some 10 million hidden hearing loss, a condition in which the audiogram is essentially normal but self-reported problems in background noise persist.
Survey Highlights Gaps and Opportunities
Overall, the results of the NHIS survey show that hearing difficulties are a prevalent condition with substantial gaps existing between the condition and referral to specialists for treatment and intervention.
For professionals these gaps represent an opportunity to build stronger relationships with primary care specialists, as well as a chance, given the low uptake of hearing aids, to better education individuals with self-reported hearing problems on the range of interventions available to them.
Reference
Mahboubu, et al (2017) Prevalence, Characteristics and Treatment Patterns of Hearing Difficulty in the United States. JAMA Otolarngology. Published online Nov 22 2017







We are approaching hearing care with better technology today. The key to better sensory processing is location of targets around us. The latest Resound Linx 3-9D, is a brilliant change that allows localization and depth of sound field available to the hearing aid wearer. The CI cannot mimic this function! This is where the natural functions of the middle and inner ears complement this radically new technology!
CI’s could be a thing of the past, except for fitting totally profound hearing losses.