 HHTM readers, we have a guest contributor this week who offers a very thorough and informative two-part blog on concussions. Dr. Peter Marincovich earned his graduate degree in communicative disorders from Louisiana State University, and his Ph.D., in Audiology from the University of Memphis. A Santa Rosa native, Dr. Marincovich has practiced in his home town since 1984, working with patients of all ages and levels of hearing loss. He is also a frequent presenter at seminars and academic conferences. His areas of special interest include the assessment of auditory and vestibular disorders, healthcare policy, hearing care solutions and delivery systems and audiology education. He holds specialized credentials in teaching the handicapped, and conducts courses at Santa Rosa Junior College.
HHTM readers, we have a guest contributor this week who offers a very thorough and informative two-part blog on concussions. Dr. Peter Marincovich earned his graduate degree in communicative disorders from Louisiana State University, and his Ph.D., in Audiology from the University of Memphis. A Santa Rosa native, Dr. Marincovich has practiced in his home town since 1984, working with patients of all ages and levels of hearing loss. He is also a frequent presenter at seminars and academic conferences. His areas of special interest include the assessment of auditory and vestibular disorders, healthcare policy, hearing care solutions and delivery systems and audiology education. He holds specialized credentials in teaching the handicapped, and conducts courses at Santa Rosa Junior College.
Knowing the Signs and Symptoms Linked to
Traumatic Brain Injury (TBI) Can Save Lives
By Dr. Peter Marincovich, Ph.D.
The biographical sports film “Concussion” raised public awareness of Traumatic Brain Injury (TBI) by turning the media spotlight on brain damage suffered by Pittsburgh Steelers Center Mike Webster during his football career, a condition only discovered during an autopsy after he was found dead in his pickup truck.
Recently, the specter of TBI was raised again by soccer icon Brandi Chastain, who revealed that she suffered two concussions while playing in college. Realizing that more research is needed, Brandi Chastain, along with Olympic swimming standout Jenny Thompson and Cindy Parlow Cone — one of Chastain’s teammates on the Women’s U.S. National Soccer team — have all agreed to donate their brains for concussion research when they pass away.
TBI is a significant public health concern and a major cause of permanent disability. This condition can impact the physiology, cognition, hearing loss, emotional regulation and social interactions of an individual, with long-term outcomes ranging from complete recovery to disability and death, according to the National Institute of Neurological Disorders and Stroke (NINDS).1, 2
This overview is offered as a guide to physicians, educators and other professionals when making recommendations to individuals with TBI and their caregivers. It briefly covers what is known about brain changes that occur in the wake of a TBI incident, and discusses recent advances in cognitive remediation strategies that can be applied in connection with one specific TBI outcome — hearing loss. 3
Statistics
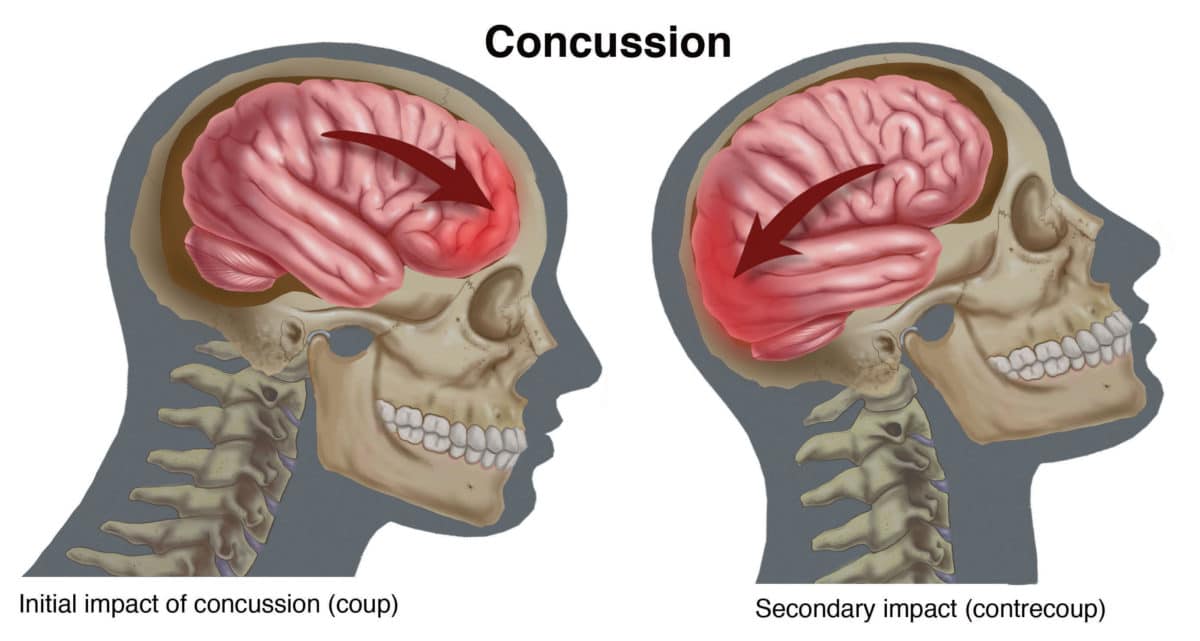
Traumatic brain injury (TBI) is caused by a blow or jolt to the head, or by a penetrating head injury that disrupts the normal function of the brain. Each year in the United States, at least 1.7 million TBIs occur, either as an isolated injury or in combination with other injuries, based on Centers for Disease Control (CDC) reports.4
It is believed that these reports are low, due to the fact that many “mild” TBI cases are treated outside of hospital rooms in doctors’ offices and military facilities. Other less severe cases of TBI may go completely unreported, especially if the injured person does not recognize and report symptoms.5
Causes
According to the CDC, the leading causes of TBI are falls (35%), motor vehicle accidents (17.3%), when a person is struck by or against something (16.5%), and assaults (10%). Falls cause 50% of TBIs among children aged 0-14, and among adults aged 65 years and older.
While motor vehicle accidents are the second leading cause of TBI, they make up the largest percentage of TBI-related deaths (31.8%). The very young (four years and younger) and adults over 75 have the highest risk of TBI, with males diagnosed more frequently (59%) than females.
Military personnel returning from combat in Iraq and Afghanistan have been profoundly affected by TBI with an estimated one in five soldiers experiencing a head injury, including blast-related trauma.
According to data published by the DVBIC, The Defense and Veterans Brain and Injury Center, the total number of service members with TBI diagnoses has more than doubled in the past five years with the majority categorized in the mild and moderate categories. Consequently. 6,7,8
In the sports world, it is estimated that a pro football player will receive an estimated 900 to 1,500 head blows during a season, making football a sport with a 75% chance of concussion for men, while soccer is the most common sport with a 50% chance of concussion for women. The impact speed of a football player tackling a stationary opponent is 25 mph, while the impact of soccer ball being headed by a player is 70 mph.89,10
In part two we will explore warnings signs associated with TBI, what a person should do if he or she suspects that concussion has occurred, how to communicate with a suspected TBI victim during the assessment process as well as how to work with, or teach, those who have had such an injury.
Feature Image courtesy of Compel Visuals
References:
- NINDS: National Institute of Neurological Disorders and Stroke. (2016) Traumatic Brain Injury: Hope Through Research.
- Janet Brown, Brainline.org article, 2009. “Hearing Loss After TBI – Physical Symptoms of Brain Injury” published online.
- Kinnunen, K.M., Greenwood, R., Powell, J.H., Leech, R., Hawkins, P.C., Bonnelle, V., Patel, M.C., & D.J Sharp. (2010) White matter damage and cognitive impairment after traumatic brain injury. Brain: 134: 449-463
- CDC: Centers for Disease Control and Prevention. (2013) Traumatic Brain Injury Statistics.
- Unreported TBI, concussions: American Medical Society for Sports Medicine position
- Warden, D. (2006) Military TBI during the Iraq and Afghanistan wars. J. Head Trauma Rehabilitation. 21(5):398-402.
- Okie, S. (2005) Traumatic brain injury in war zones. N. Engl. J. Med. 352(20): 2043-2047.
- Defense and Veterans Brain Injury Center.
- Sports Concussion Institute – “Concussions are a Fact of Life in Today’s Sports World,” 2008-2012.
- McKeag, DB et al. “Summary of Evidence-Based Guideline Update: Evaluation and Management of Concussion in Sports,” a report of the Guideline Development Subcommittee of the American Academy of Neurology. Published online March 18, 2013, before print edition June 11, 2013, Vol. 80 No. 24.