“Signal & Noise” is a bimonthly column by Brian Taylor, AuD.
Segmentation is a powerful tool to better understand what the marketplace values. Perhaps more importantly, from the perspective of the business manager, segmenting demographic data sheds light on gaps in the market that can be turned into opportunities for those with entrepreneurial spirit.
We know, for example, when we segment hearing aid use by degree of hearing loss we can uncover opportunities to better meet the needs of 90% of those with mild to moderate high frequency hearing loss – a segment which comprises approximately three-quarters of the entire American hearing impaired population.
Segmenting Age Groups to Better Meet Their Needs
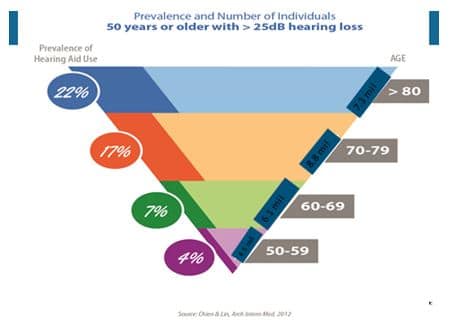
The same approach can be used when we segment hearing aid use by age. Chien and Lin (2012) used data from the National Health and Nutritional Examinations Surveys (NHANES), collected between 1999 and 2006, to examine the prevalence of hearing aid users among American adults aged 50 and older. Although their findings should not be surprising (yes, individuals over the age of 80 are more likely to wear hearing aids than adults under the age of 70), upon closer inspection we can begin to tease out some valuable insights on how we can collectively better serve the needs of all our patients.
A summary of their epidemiological work is shown in Figure 1. Chien & Lin (2012) estimated that 14.2% (3.8 million) individuals in the U.S. who are 50 years or older with hearing loss wear hearing aids. Note in Figure 1 that 22% of adults aged 80 and above with hearing loss use hearing aids, while 4.3% of individuals between the ages of 50 to 59 with hearing loss use them. Thus, the prevalence of hearing aid use essentially doubles with every decade of age.
The Value of Segmentation in Epidemiological Data
The real question is, how can we use this information, collected from a large representative sample of the U.S.?
Professional Imperative Spelled out by Low Uptake
First, the data tell us that the overall rate of hearing aid use is remarkably low, especially for adults under the age of 70.
It is imperative for the entire industry to read, understand, and then begin to share the peer reviewed literature (see Table 1), much of it published in the past three years, with other medical professions, especially primary care gatekeepers.
Our scientifically-defensible message needs to be that hearing loss of adult onset is not an inconsequential aspect of the aging process. Taken one step further, the overall low uptake of hearing aids necessitates the need to stay politically engaged, so that hearing rehabilitation services, including hearing aids become reimbursable by health insurance. Of course, this is no easy feat. It requires us to collect data to support the effectiveness of various treatment approaches, and we all know collecting data (i.e., measuring outcomes of our treatment recommendations) is something anathema for many hearing care professionals.
Table 1. Recently published scientific evidence supporting the association between age-related hearing loss and other medical conditions.
| 1. Lin et al (2013) Hearing Loss and Cognitive Decline in Older Adults JAMA Int Med. 173, 4.
2. Fisher et al (2014) Impairments in Hearing and Vision Impact on Mortality in Older People. Age and Aging. 43,1. 3. Mick et al (2013) Association between Hearing Loss and Social Isolation in Older Adults. Otolaryngol-H& N Surg, 150, 378-384. 4.Chuan-Ming. L. (2014) Hearing Impairment with Depression in US Adult Populations, NHANES 2005- 2010. Otolaryngol-H&N Surg. 140, 4. 5. Lin et al (2014) Association of hearing impairment with brain volume changes in older adults. Neuroimage. 40, 84-92. 6.Kamil et al (2014) Association between Hearing Impairment and Frailty in Older Adults. J Am Geriatrics Soc, 62, 6. 7. Foley et al (2014) Association between Hearing Loss and Healthcare Expenditures in Older Adults. J Am Geriatric Soc, 62, 6. 8. Genther, D. et al (2015) Association between Hearing Impairment and Risk of Hospitalization in Older Adults. J Am Geriatric Soc. 63,6. |
On a side note, pay close attention to the writings of Professor Barbara Weinstein of the CUNY Graduate Center, many of which will begin to appear at HHTM.
Practice Differently for Differences in Hearing Aid Use
Second, when we carefully examine differences in hearing aid use for various age groups it provides valuable insight into how we can begin to practice differently.
We desperately need to search for effective alternatives to traditional hearing aids to expand the appeal of audiological services.
Let’s take the oldest group from the NHANES data, those aged 80 and above. Twenty-two percent of this group with hearing loss use hearing aids. Even if we double the number of hearing aid users within the oldest cohort, we still have not managed to fit hearing aids on half of the age group that has the highest prevalence of hearing loss.
When one considers all of the other co-morbidities affecting this group, such as dementia and other physical conditions which make it difficult to use hearing aids, we begin to see the need for alternative treatment approaches if we truly want to reach this group of people. These alternatives are likely to include directed audio solutions{{1}}[[1]]Disclosure: I am employed by a company bringing one type of this product to market[[1]], coaching communication skills and brain training exercises.
As more of these approaches are brought to market we need to demand these alternative treatments are supported by good evidence from well-designed clinical studies.
Things We Can Do Right Now
Providing efficacious treatment options takes time and money, so what can we do today to help improve hearing aid uptake among this group of older patients? Part of the answer to this question rests with our ability to provide better, more efficient follow-up care.
- A 2013 study from Finland, which sampled 249 hearing aid users over the age of 70 found that 55% used their hearing aids full time, 27% used them less than 6 hours per day and 11% never used their hearing aids. Non-use of hearing aids increased with advancing age, as approximately 25% of 75-80 years olds were non-users, while almost 50% % of 85 years and older were not using their hearing aids. This finding suggests other cognitive and physical factors make the routine use of hearing aids difficult and necessitates that hearing care professionals search for other courses of action to improve daily communication among this group.
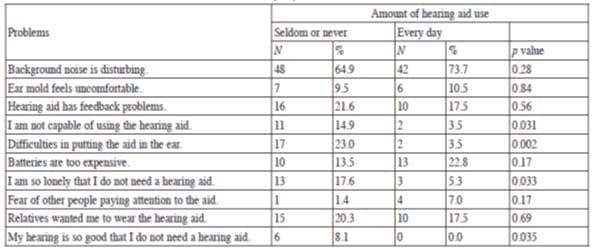
A more careful examination of the problems experienced by elderly users (aged 70 and older) warrants serious consideration.
- Table 2 below, which was taken from the Finnish study comparing hearing aid problems between those classified as non-users and every day hearing aid users, is worthy of consideration. Note that for many of the problems cited by both groups there are not significant differences between groups. For example, “background noise is disturbing” was mentioned as a problem by 65% of non-users and 74% of every day users and “feedback problems” was cited by 22% of non-users and 18% of full-time users, respectively. On the other hand, issues related to loneliness, self-confidence and physical conditions making insertion of hearing aids into the ears difficult were clearly more of a problem for non-users compared to their similarly aged full-time users.These findings suggest that better, more sophisticated hearing aid technology is probably not the answer. Rather, taking the time to master personal adjustment counseling would be a viable way to improve hearing aid use among patients aged 70 and older. Clearly, such as approach takes more precious clinical time and is unlikely to result in better reimbursement, but it does present opportunities for our profession to meet the unmet needs of a certain segment of the population.
Table 2. Comparison of problems experienced by elderly hearing aid users in Finland. The two groups compared are non-users and full-time users. From Salonen, et al (2013) Hearing aid compliance in the elderly. B-ENT. 9, 23-28.
Our Evolving Role as Hearing Healthcare Providers
When we consider how important at-home activities such as television watching and being able to fully participate in a common family activities, we should begin to realize that our primary role is not to dispense hearing aids, but to match the proper technology and “therapy” to the daily functional needs of the individual.
Fortunately, we live in age where the morphing of customizable medical devices and cool, gadget-like consumer electronics allow us to provide our patients, even octogenarians, with choices beyond traditional hearing aids. It’s up to forward thinking audiologists and hearing instrument specialists to embrace them. This starts by carefully considering how these hybrid alternatives fit into the revenue-generating, bread and butter activities of hearing aid selection and fitting.
The segmentation data shows opportunities to grow the demand for our services, if we can provide value to untapped markets. Actually putting this into action means we have to swim upstream against the inertia of limited clinical offerings, public indifference to the consequences of hearing loss of adult onset and antiquated reimbursement methods. Let the dialogue begin.
Part 2 of this article will address hearing loss in individuals under the age of 70.
Brian Taylor, AuD, is Senior Director, Clinical Affairs, for Turtle Beach/Hypersound. He continues to serve as Editor of Audiology Practices, the quarterly publication of the Academy of Doctors of Audiology. During the first fifteen years of his career, he practiced clinical audiology in both medical and retail settings. Since 2005, Dr. Taylor has held a variety of leadership & management positions within the hearing aid industry in both the United States and Europe. He has published over 50 articles and book chapters on topics related to hearing aids, diagnostic audiology and business management. Brian has authored three text books: Fitting and Dispensing Hearing Aids (co-authored with Gus Mueller), Consultative Selling Skills for Audiologists, and Quality in Audiology: Design & Implementation of the Patient Experience. His latest book, Marketing in an Audiology Practice, was published in March, 2015. Brian lives in Golden Valley, MN with his wife and three sons. He can be reached at [email protected] or [email protected].
feature image courtesy of Cambridge in Color