“Signal & Noise” is a bimonthly column by Brian Taylor, AuD.
Identifying and addressing the unmet needs of people with hearing loss means more than reducing costs (the Public Health Perspective) or improving devices (the Biomedical Perspective). The extent and limits of those approaches were covered in part 1. Today’s post suggests that we can meet people’s hearing needs better if we hand them the reins.
The Psychosocial Perspective
Aside from cost effects on hearing acceptance statistics, reports indicate low uptake may be the result of psychosocial factors, which are often overlooked. Recent studies suggest several factors, other than cost, associated with seeking help for hearing loss.
A 2014 retrospective study involving 307 adults aged 60 and older found that among the factors influencing help seeking for hearing loss were a declining ability to cope with hearing loss, greater levels of self-reported difficulties and social pressure to take action. Other research suggests that passive acceptance of hearing loss, stigma and the negative outlook of others with respect to hearing aid use may delay help seeking for those with a possible hearing loss.
Experts in the field point out seeking the assistance of a hearing care professional about a potential hearing loss should not be equated with a willingness to purchase hearing aids. In fact, a 2012 peer reviewed study suggested that when given a choice of interventions, some of which do not center on the provision of a device, about 40% of patients opt for the non-device option. Further, given that approximately 80% adults with hearing loss do not seek help during the first 50 to 10 years after noticing hearing loss suggests that beyond the introduction of lower cost technology, in-depth patient counseling and education are important considerations in solving the problem of the long delay in help seeking and use of hearing aids.
Time to Leave the Biomedical Model and Let Patients Set the Agenda
Regardless of your stance on the PCAST report and the underlying factors contributing to delays in seeking help and the poor uptake of hearing aids, clinicians would be wise to use more patient-centric communication. It would help the entire profession move beyond the limited, and perhaps stagnant, biomedical perspective that too often thinks all hearing difficulties can be solved with a better hearing aid or a more remarkable service experience with the professional.
At the same time, genuine patient-centric communication, which is a hallmark of the psychosocial perspective, would address the serious shortcomings of public health officials who believe the problem can be solved with a cheaper device sold directly to consumers. Today, early intervention and patient-centered communication, in which the patient is allowed to set the agenda is, as Shakespeare said, “more honored in the breach than the observance.” For example, Grenness and colleagues reported in a 2015 issue of JAAA that an astounding 83% of all information given by the audiologist throughout the patient consultation is biomedical in nature: we love to discuss the audiogram and hearing instrumentation.
As more Baby-boomers, who typically have a strong desire for direct involvement in their healthcare, enter the market for our services it is important we peel Harvey Abram’s onion and recognize their “stage of change” and “triggers to action”. Additionally, clinicians need to recognize that the vast majority of hearing loss in adults starts within the normal range and deteriorates slowly. We need to use technology to engage people early through self-screening and adaption of technology that helps in specific listening situations, which are often problematic for aging individuals with “normal hearing for their age.”
For those that adhere to a purely biomedical perspective, alternative interventions designed to help patients with essentially normal hearing or mild loss can be viewed as gateway products that may speed the journey to traditional hearing aid acceptance as a patient ages and needs more help.
Five Reasons Patients Seek Hearing Help
Recently, leading researchers, such as Gaby Saunders, Arlene Carson, Louise Hickson and Arianne Laplante-Levesque have begun to popularize the use of various models to describe the behaviors and attitudes associated with the chronic condition of age-related hearing loss. We can begin to infuse their work into our counseling approach with patients by addressing five key reasons why individuals, often waiting several years, finally decide to seek help from a hearing care professional. (By the way, none of these reasons have anything to do with cost). According to the experts the five reasons are:
- Have a support network (family, friends, trusted family doctor) who encourage them to seek assistance
- Have more severe symptoms (greater hearing loss)
- Current ability to cope with their condition is ineffective
- Does not expect to be stigmatized (judged, mocked or belittled) for seeking help
- Feels the condition has a significant impact of daily living
In a nutshell, these five areas of concern are known as the Health Belief Model. It is an essential part of our job to address each of these points during the face-to-face consultation with a patient, or in our interactions with the community. In the clinic, we can accomplish this by shifting from one-way dialogue about test results and technology to give-and-take conversations that unpack the emotional baggage associated with living for so long with a debilitating condition. Perhaps if we focused on counseling & intervention strategies that addressed these five areas, uptake for our products and services would be higher:
- Encourage early self-screening of hearing loss. Educate the community that even adults with normal audiograms may have difficulties with day-to-day communication, and intervention – beyond traditional hearing aids – can be helpful.
- Embrace the public health perspective through the judicious use of PSAPs and other hearables for patients with milder self-reported hearing difficulties. It also includes the use of community-based health workers to educate the entire population about the importance of hearing screening, the deleterious effects of hearing loss of adult onset and effective early intervention options.
- Provide emotional support. Discuss the importance and willingness of getting help while respecting the patient’s values and “stage of change”
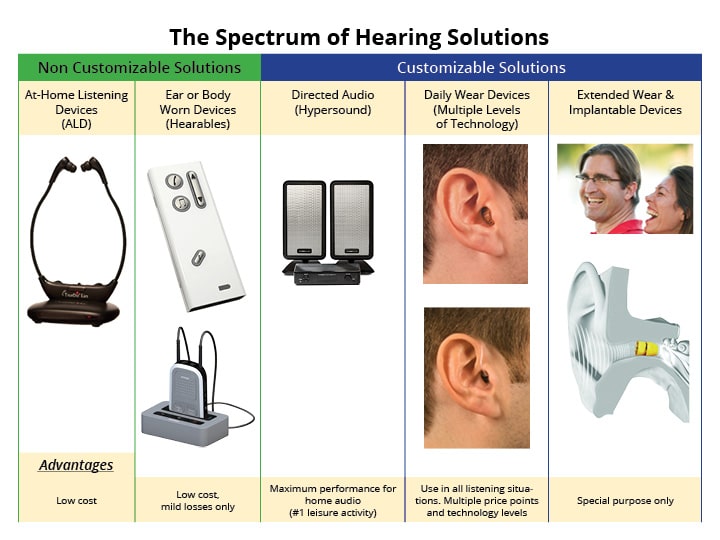
- Offer unbiased educational information. Show the patient all of their possible solutions, including the advantages and limitations of each. This can be done with a visual aid like the one shown in Figure 1.
- Conduct a hands-on demonstration of various technology offerings. Allow patients to touch, feel and use various devices prior to purchasing them. In short, modernize your ALD display with hearables.
Figure 1. An example of a product education visual aid.
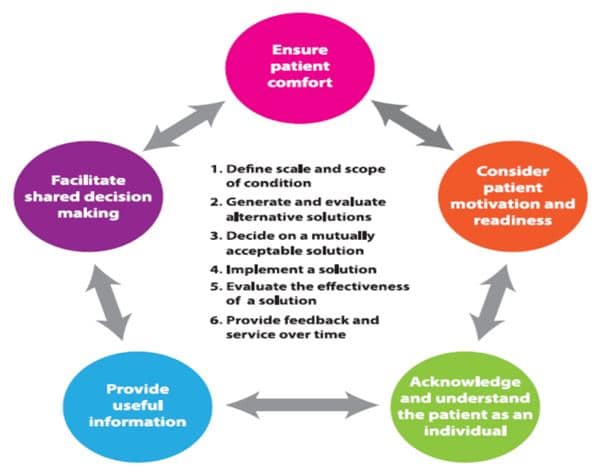
Finally, when authentic patient-centric communication and shared decision making are put into practice, as shown in Figure 2, individuals are more likely to feel that we addressed their needs and helped them – sometimes without even dispensing a product. At the end of the day it’s these humanistic communication skills, rather than our technical ability that will transcend our recent spats over the re-regulation of hearing aids.
Juggling 3 Different Perspectives
That executive panel in part 1 of this post, representing the biomedical perspective, is the clinician’s ally, but hearing care professionals owe it to their patients to broaden their perspective on how to better meet the needs of those with hearing loss and communication difficulties stemming from it.
Keep your mind open to what all individuals with communication difficulties value. It may be something no one has yet to offer. The future of our profession hinges on our ability to juggle three different perspectives. The status quo – conducting a routine audiogram and fitting hearing aids on those that after several years of passive acceptance eventually find their way to our clinics – must change. It’s time to usher in a new era of clinical audiology that embodies all three perspectives.
Figure 2. A roadmap for patient-centric communication based on the work of Laya Poost-Faroosh, Louise Hickson, Caitlin Grenness and others
Brian Taylor, AuD, is Senior Director, Clinical Affairs, for Turtle Beach/Hypersound. He continues to serve as Editor of Audiology Practices, the quarterly publication of the Academy of Doctors of Audiology. During the first fifteen years of his career, he practiced clinical audiology in both medical and retail settings. Since 2005, Dr. Taylor has held a variety of leadership & management positions within the hearing aid industry in both the United States and Europe. He has published over 50 articles and book chapters on topics related to hearing aids, diagnostic audiology and business management. Brian has authored three text books: Fitting and Dispensing Hearing Aids (co-authored with Gus Mueller), Consultative Selling Skills for Audiologists, and Quality in Audiology: Design & Implementation of the Patient Experience. His latest book, Marketing in an Audiology Practice, was published in March, 2015. Brian lives in Golden Valley, MN with his wife and three sons. He can be reached at [email protected] or [email protected].
feature image courtesy of Cambridge in Color (edit)








As always an excellent article. However, I have to somewhat degree with the assessment of a public health perspective.
I have worked in public health for 25 years, working on state, local and national projects funded by by the Robert Wood Johnson and other foundations and government. I am hearing impaired and have a consumer web site called Hearing Loss Toolkit.
Frankly, I have almost never heard hearing loss mentioned in public health discussions, including a RWJF leadership group I participate in. I think it’s pretty invisible in that sector, as it is in primary care offices.
At its best, I think a population health perspective, following the Triple Aim, seeks to improve quality, reduce cost and increase access for populations.
I haven’t followed the PCAST process closely, but I concur that it should not be based on just reducing costs. It’s a tricky one, though, because cost is an issue. I was quoted $6800 for two hearing aids a few years ago and recently found that my hearing test and adjustment (about $500) was not covered by my ACA insurance plan. I would like to see hearing related organizations band together to have a common policy message about the lack of coverage for people over 18. It’s ridiculous. Part of the issue is the societal lack of cognizance of early prevention of potential hearing decline and the link to brain health.
I would like to see audiologists as prime providers of hearing loss services, because of their expertise and I would also like to see hearing health education materials/ some sort of referral process available in PCP offices, because I think a lot of people go there first.
I’d also love to see a national consumer survey conducted by a neutral party like RWJF on hearing loss. I think there are vast #s of people who have no idea what to do about their loss, PCPs are uneducated and consumers end up going to dealers who vary in quality.
In public health, even in an oral health project in which I am now involved, we solicit extensive consumer and provider input to determine need—focus groups, surveys, key informant interviews, literature review, and review of best practices in other areas. I’d like to see holistic (not just clinical—lifestyle) hearing health consumer education that was offered in an array of formats—as in the chronic disease realm—hotline (or email lines), support groups, resource centers, coaching and advice about technology. My dream would also incorporate health literate strategies and use online and print vehicles. I think what is mentioned about emotional health is very important; I think if people had more education, they would feel less powerless. Totally concur with the idea of CHWs or hearing loss support specialists. A public health perspective can lend itself to this strategies.
Ann Conway PhD
OOPS meant “disagree” in that first line!
Brian: Always interesting reading although a following discussion might prove fruitful. A couple of points:
1. 83% of information discussed with patients following evaluation is “biomedical”? If this is true, just what is being discussed? The audiogram? And who is doing all this discussion? About 90% of the things discussed following an annual physical checkup is “biomedical”. What’s the difference between “their” discussion and “ours”?
2. We are always quick to eliminate costs, yet sales data seems to show that essentially the same instruments available through big box stores at less cost is the most rapidly growing segment of the HA industry. If cost is not a major consideration, why do people seek these sources for help? And,does this really tend to suggest that more of a “sales pitch” in the patient follow-up should replace the “biomedical” explanations?
3. If billing issues have arisen from lack of reimbursement for audiology’s usual “bundled” Tx services, just how do we bill legitimately for emotional therapy, education about PH services, and other typically “non-diagnostic” interventions. Most audiologists cannot even get paid for Tx that was incorporated into their training.
Audiology is facing some difficult times. Many agree with you about the need to modify what we provide. How audiology makes what changes deserves lots of discussion. Thanks for starting it.
Mike
I enjoyed this article and agree with so much of what is being said. However, as someone with hearing loss who also works in the hearing industry I think the system is broken. Lack of insurance coverage of a hearing solution is a great challenge to everyone involved. As a patient, it’s so frustrating to have insurance cover the evaluation to verify that you absolutely have hearing loss and then be unwilling to cover anything to help you. As a patient, when you go to get an evaluation by an audiologist you know that they make their money by representing certain brands and types of hearing aids and selling hearing aids is how they make their living. In fact, in many cases determining how many hearing aids can be sold to that person over a period of time is really important to their bottom line. By going to an audiologist I won’t learn anything about implantable options, unless my loss is too profound for them to help, and they refer me to a cochlear implant. This leaves the consumer (me in this case) very guarded. I know I am not being told about everything. I just took a test that reminds me of how horrible my hearing is, I’m being told good things about the brands they carry and not good things about the hearing aids or therapies they don’t work with. I can’t fathom having “emotional therapy” with someone who’s goal is to try to sell me something. I have had many audiologists in my lifetime, very few have taken my own lifestyle into account. Therefore, I go on the internet and I find out what my options are by doing my own research and learning what people are paying for different devices. I learn about surgical procedures, hearing aids and amplifiers. I speak with other patients on message boards. My interest is how well I hear in life, not in a soundproof booth. I wish I had more answers. The consumer perspective however, I had 30 years of experience on that side!
Thanks for addressing this important topic. At the Ida Institute, we have worked with patient-centered care for years and understand it as healthcare that is designed around the patient’s preferences and values, involves the patient’s family and friends, reinforces shared decision-making and goal setting and prioritizes the free-flow of information. Better understanding of the needs and wishes of the patient, and incorporating their needs into the rehabilitation process can help increase patient satisfaction, encourage patient collaboration, and help lead to better outcomes.
Despite research supporting the benefits of patient-centered care, many hearing care professionals report that they feel unprepared to adopt counseling and other methods in their daily practice. They need resources and practical tools to help them integrate patient-centered principles in their practice.
In collaboration with our global community, Ida Institute has created a suite of easy-to-use tools that provides a method and structure to open communication, uncover motivation and engage patients in the self-management of their hearing loss. The Ida Tools can help audiologists implement patient-centered care principles in their own clinical practice. And it does not have be more time-consuming – which seems to be a common misconception.
All of our tools can be freely downloaded from our website http://www.idainstitute.com .
Lise Lotte Bundesen