Hearing Healthcare Market Development Column
The question as to whether the telehealth model provides the same quality of care as the traditional face-to-face model in hearing healthcare is topical given that the coronavirus pandemic has entered a third wave. Auditory Insight’s analysis shows that the model created by the telehealth hearing aid company, Listen Lively (Lively), is closing the quality of care gap relative to face-to-face.
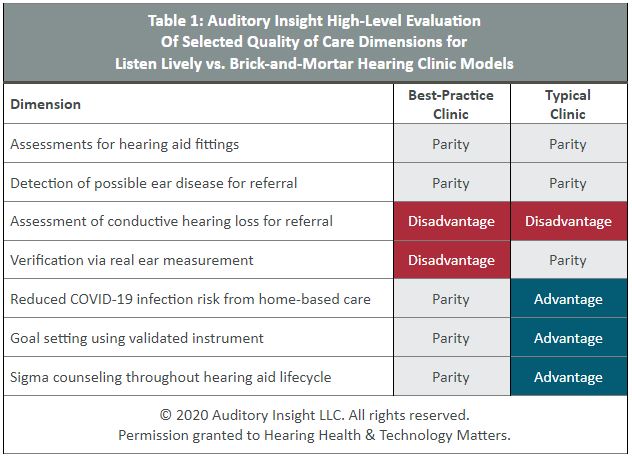
Auditory Insight has evaluated how the quality of care provided by the Lively model compares to two types of brick-and-mortar hearing clinics, one that employs clinical best practices, and one that is typical of the norm. See Table 1 below.
We chose to benchmark Lively because the company sets the gold standard in replicating the clinical face-to-face (F2F) model remotely and digitally. Lively’s model is unique, deploying a combination of hearing aids programmed with the patient’s unique profile, a video welcome call with an audiologist, and a robust goal setting program.
Assessments for hearing aid fittings and detection of possible ear disease for referral
Compared to both the best-practice and typical clinic models, the Lively model’s quality of care is at parity along these two dimensions. The company relies on an online hearing test to generate patients’ hearing profile for programming hearing aids.
In order to detect possible ear disease, Lively requires patients, before receiving their hearing aids, to complete the Consumer Ear Disease Risk Assessment (CEDRA), a validated questionnaire with a false negative rate of 10%. Those patients who create a flag on the CEDRA, or earlier during the online hearing test, must speak with an audiologist on a video call to determine the need for a referral for a full hearing exam.
Assessment of conductive hearing loss for referral
Almost all audiologists conduct pure-tone air and bone conduction audiometry—tests sufficient to rule out the presence of conductive hearing loss—as noted by Traynor and Hall. Bone conduction audiometry requires the patient’s presence in the clinic, and as of this writing, Lively does not use the antiphasic and diotic digits-in-noise testing, advocated by Swanepoel and Hall, to detect conductive hearing loss remotely. Thus, the Lively model’s quality of care is at a disadvantage relative to both the best-practice and typical clinic in identifying possible conductive hearing loss for referral.
However, Lively does refer patients based on flags in the CEDRA and patterns in their online hearing test. In addition, the company recently piloted a video otoscopy program, according to Christina Callahan, Lively’s director of clinical audiology.
Verification via real-ear-measurement
Real-ear-measurement (REM) verifies a hearing aid’s prescription by placing a probe microphone into the ear canal while the patient is wearing their hearing aids. The patient must be present in the clinic in order for the audiologist to conduct REM. Thus, compared to the best-practice clinic which regularly conducts REM, the Lively model’s quality of care is at a disadvantage.
Yet, how many audiologists actually conduct REM? “Despite the documented benefits of conducting REM during hearing aid fittings and best-practice recommendations by a number of professional bodies, only 57% of respondents own REM equipment,” asserted Amlani et al. Moreover, “a mere 34% of respondents reported using the equipment consistently.” Compared to the two-thirds of clinics who do not conduct REM, Lively’s care model is at parity.
Reduced COVID-19 infection risk from home-based care
One of the clear benefits of telehealth is that it eliminates patients’ risk of COVID-19 infection from visiting a hearing healthcare clinic in-person. As in the case of the use of REM for verification, the use of telehealth varies by clinic. In the Hearing Review’s COVID-19 Impact Survey #3, just under half of clinics reported that telehealth was part of their strategy in dealing with the pandemic, with most of those clinics leveraging tele-audiology for hearing aid adjustments, as well as follow-ups and counseling.
However, only 4% of clinics reported using telehealth for audiological evaluations. Thus, along this dimension, the Lively model’s quality of care is at parity with the small proportion of clinics that use telehealth for all patient interactions. Relative to the remaining clinics, Lively’s care model has an advantage.
Goal setting using validated instrument
Auditory Insight analysis shows that only 70% of hearing aid owners wear their hearing aids on a regular basis. As a result, best practices include a goal setting program based on a clinically validated instrument such as the Client Oriented Scale of Improvement (COSI), a clinical tool developed by the National Acoustics Laboratories (NAL) to document patients’ needs and measure improvements in hearing ability.
“Most audiologists conduct, at a minimum, some cursory goal setting with patients. For instance, the audiologist may ask about telephone use or communication in noisy listening situations,” reported Dr. Brian Taylor, AuD, director of scientific and project marketing at Signia, in an email interview. Taylor clarified, however, that “very few audiologists appear to have a systematic way of documenting how individuals are functioning and what strategies and technology they may benefit from over an entire range of daily activities.”
In contrast, Lively has COSI goals on file for 98% of their consumer-patients who complete the orientation call. During each subsequent interaction, Lively audiologists follow up on patient goals and track any changes. Hence, along the goal-setting dimension, the Lively model’s quality of care is at parity with a best-practices clinic and enjoys an advantage over the typical clinic.
Stigma counseling throughout the hearing aid lifecycle
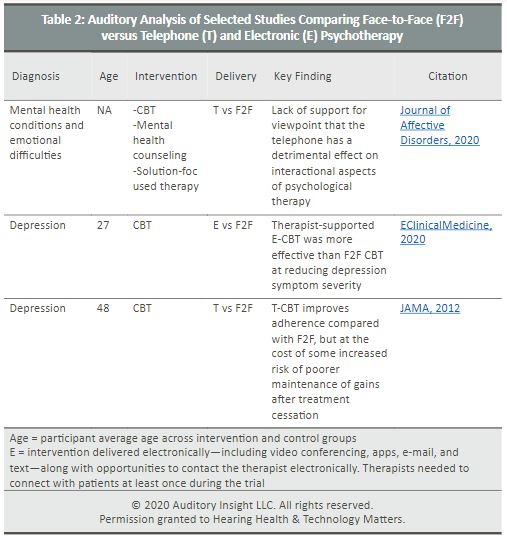
Lively addresses consumer-patient concerns about stigma when they surface during goal-setting conversations, as do brick-and-mortar clinics who systematically conduct goal-setting programs. This column’s July 2020 profile of Lively asserted that the company’s inability to provide F2F stigma counseling was a disadvantage of its care model. Support for that viewpoint came from a 2012 JAMA article which found that therapy administered over the telephone improves adherence compared with F2F therapy, but at the cost of some increased risk of poorer maintenance of gains after treatment cessation. (See Table 2 below.)
The JAMA article examined the efficacy of telephone vs F2F cognitive behavioral therapy (CBT). CBT is a common type of psychotherapy or talk therapy often used to help people manage stressful life situations. Auditory Insight believes CBT is the optimal framework for stigma counseling because the loss of confidence, even shame, engendered by stigma impacts people’s thoughts, emotions, and behaviors, cornerstones of CBT.
Since the Lively profile, Auditory Insight has updated its point of view to assert that the Lively model’s quality of care is at parity with best-practice clinics and holds an advantage over typical clinics, along the dimension of stigma counseling. That update stems from two new meta-studies published in 2020, one of them in June, shown in Table 2 below. The EClinicalMedicine study is of particular interest because it examined the efficacy of E-CBT, interventions including video conferencing, apps, e-mail, and text. Although the study participants’ average age of 27, with some children, make the study less relevant for hearing healthcare, the finding that E-CBT was actually more effective bears watching.
References:
- Are there interactional differences between telephone and face-to-face psychological therapy? A systematic review of comparative studies. Journal of Affective Disorders. Volume 265, 15 March 2020, Pages 120-131 https://www.sciencedirect.com/science/article/pii/S0165032719319743?via%3Dihub
- A comparison of electronically-delivered and face to face cognitive behavioural therapies in depressive disorders: A systematic review and meta-analysis. EClinicalMedicine. Volume 24, 100442, JULY 01, 2020. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30186-3/fulltext
- Effect of Telephone-Administered vs Face-to-face Cognitive Behavioral Therapy on Adherence to Therapy and Depression Outcomes Among Primary Care Patients. JAMA. 2012;307(21):2278-2285. doi:10.1001/jama.2012.5588
 Nancy M. Williams is President of Auditory Insight, a boutique consultancy advising leaders on transforming hearing healthcare. Nancy partners with senior leaders of pharma and device companies to develop successful commercialization strategies based on deep insight into patient needs, practical understanding of clinical behaviors of audiologists and ENTs, and unique viewpoints on how hearing healthcare is evolving. She holds an MBA from Harvard Business School and a B.A. from Stanford University in Quantitative Economics, both with distinction.
Nancy M. Williams is President of Auditory Insight, a boutique consultancy advising leaders on transforming hearing healthcare. Nancy partners with senior leaders of pharma and device companies to develop successful commercialization strategies based on deep insight into patient needs, practical understanding of clinical behaviors of audiologists and ENTs, and unique viewpoints on how hearing healthcare is evolving. She holds an MBA from Harvard Business School and a B.A. from Stanford University in Quantitative Economics, both with distinction.
**featured image courtesy Lively






