by Harvey B. Abrams, Ph.D.
In her thoughtful and thorough review of the Lively Hearing delivery model, Nancy M. Williams, HHTM columnist and President of Auditory Insight, identifies a number of Lively’s strengths which include a “patient engagement best practice” of presenting test results in a meaningful way; requiring prospective clients to complete the Consumer Ear Disease Risk Assessment (CEDRA) questionnaire; and administering the Client Oriented Scale of Improvement (COSI) to identify and articulate patients’ needs and measure their self-perceived attainment of treatment goals.
However, Ms. Williams identifies Lively’s lack of in-person interactions as a shortcoming, as such interactions, as they typically occur in traditional brick-and-mortar clinics, are “helpful for sensitive discussions, particularly relevant for those outstanding audiologists who make the time to help their patients overcome stigma and integrate hearing aids into their personal and professional lives.”
This is an interesting point and one which we want to explore further. The assumption, here, is that, given an outstanding clinician, the in-person interaction is inherently superior to an interaction conducted remotely via video. In fact, the research does not support such a position; nor do the experiences of our audiologists or the thousands of clients we’ve served.
A Review of the Research Comparing Patient Preferences for Face-to-Face (F2F) vs. Virtual Video Visits (VVV)
There is a considerable literature concerning patients’ perception of telehealth across many different quality, convenience, clinical outcome, and cost domains. In response to the assumption that F2F visits are superior to VVVs in terms of the quality of the interaction, we are focusing on a sample of studies or parts of studies that report on the quality of the communication or the overall quality of the visit.
Some 15 years ago, when telemedicine was just beginning to experience modest growth, Eikelboom and Atlas (2005) surveyed 116 patients between the years of 2004 and 2005 who had never had experience with telemedicine; in fact, 75% of those surveyed hadn’t even heard of the term “telemedicine”.
The most common reasons some (42%) of respondents reported that they would be willing to use telemedicine were the perceived reduction in waiting time for an appointment and perceived reduction in cost. The most common reason for not wanting to use telemedicine (reported by 30% of the respondents) was their preference for F2F visits (although none of the respondents had any experience with telemedicine at this time).
Fast forward a few years where Agha and colleagues (2009) compared the impressions of 221 patients who received either F2F or VVVs. Satisfaction with communication, clinical competence and interpersonal skills were rated equally for F2F and VVV.
Kruse and colleagues (2017) conducted a systematic review and narrative analysis of telehealth and patient satisfaction across 19 domains (e.g. ease of use, improved outcomes, reduced cost, etc.). Among the 51 studies included in the analysis, 9 separate studies reported “improved communication” and 5 reported “quality” as reported benefits of telehealth. Donelan and colleagues (2019) examined patient and clinical experiences with telehealth for follow-up care. The investigators found that 62% of patients and 59% of clinicians reported no difference in the overall quality of their visits.
In terms of audiology-specific telehealth applications, Gladden and colleagues (2015) surveyed 197 veterans who receive teleaudiology care through the VA. On a scale of 1-5 where 1 represents “strongly disagree” and 5 represents “strongly agree” the average rating to the question, “My relation with the clinician was the same during this session as it was in person” was 4.77.
Figure 1 illustrates the mean scores as a function of each of the 12 survey questions.
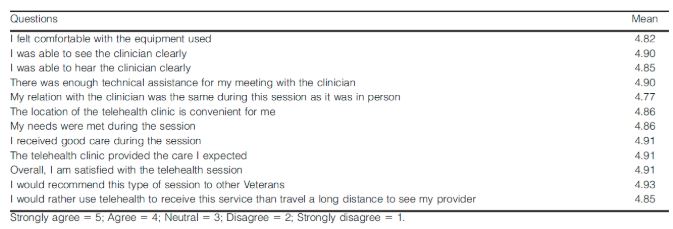
Figure 1. Survey questions and mean scores from Gladden et al. (2015)
The Lively Client Experience
As the entire client journey at Lively is remotely delivered, including our initial and follow-up appointments, we have no empirical data comparing our clients’ preference of VVVs to an alternative F2F experience.
However, we can point to some proxy information and other data that support the position that the quality of our provider-client interactions is at least as good as, and arguably better than, a F2F encounter in a brick and mortar clinic due, in large part, to the unique model that we’ve created. Some features of that model include:
- The audiologist-client relationship begins after the hearing aids have already been purchased (the audiologist never deals with price or financing issues)
- The initial orientation including “what’s in the box”, downloading the hearing aid app, downloading the virtual meeting application, and establishing the Bluetooth connection, is managed by trained customer support staff on the day the hearing aids arrives at the client’s home (minimizing the “tech support” role of the audiologist).
- We supplement the initial VVV with digital content throughout our clients’ hearing journey, including “getting started guides” for the app and hearing aids, what to expect, best practices, and more; i.e., we provide care and support through as many channels as possible.
- The initial consultation takes full advantage of the audiologists’ clinical expertise – establishing a therapeutic relationship and assisting the client with identifying their communication needs and establishing treatment goals – and following up with the client at 2 weeks, 1 month, 3 months, and 6 months
- We provide 3 years of unlimited care – meaning clients can follow-up with the customer support team or audiologists as many times as they’d like without any additional fees
Feedback from hundreds of our clients provide a convincing argument for the quality and value of our virtual interactions. A few examples of client comments that specifically reference their virtual experience include:
- Absolutely flawless product and the Zoom Doctor’s Appointment is the best thing going.
- Just recently bought one of their hearing aids. It followed a very thorough yet convenient on-line hearing test. That was followed by a couple of on-line video conferences with a doctor of audiology in which all my questions were answered and my new hearing aid was fine-tuned and adjusted for perfect effect.
- I am not only pleased with my Lively hearing aids—the best I have ever used—but also the excellent follow-up from the audiologists
- The virtual visits with the audiologist have been helpful in making slight adjustments in the volume I needed. She has also clearly explained every aspect of how to use the hearing aids and the app.
- I have had 2 on-line meetings with my Lively audiologist to have all my questions answered. I cannot imagine a better way to buy a hearing aid.
- The on-line support is first class. Much better than the doctor I first went to in person. Bottom line, I’ve never been so happy with a product.
An important proxy for overall client satisfaction (which, necessarily, includes the quality of the provider-client interaction) is Lively’s Net Promoter Score (NPS). The NPS is a measure of a company’s customer relationships based on the response to a single question: “How likely is it that you would recommend our company/product/service to a friend or colleague” as scored on a 1-10 scale.
NPS is calculated by subtracting the percentage of responders who are “Detractors” (a score of 0-6) from the percentage of responders who are “Promoters” (a score of 9 or 10). The scores can range from -100 to +100. Figure 2 illustrates an interpretation of those scores.

Figure 2. Interpretation of NPS scores
Lively’s NPS score for the first five months of 2020 is 77, which is almost 3X the healthcare industry’s average of 27. Figure 3 illustrates a comparison of Lively’s NPS with some well-known brands.
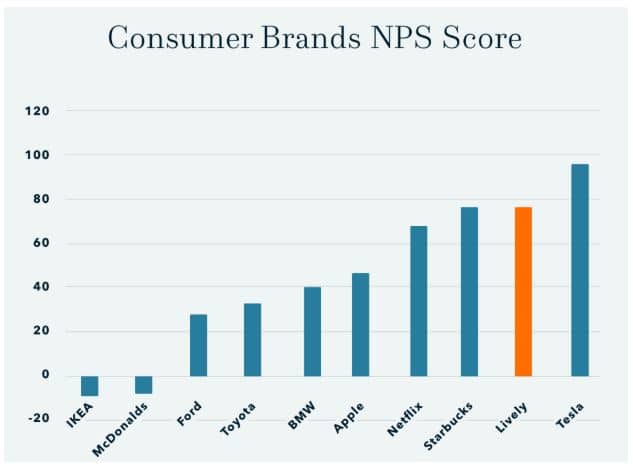
Figure 3. Comparison of Lively’s NPS score with some well-known consumer brands.
The Lively Clinician Experience
The quality of Lively’s provider-client relationship benefits the clinician as well as the client; indeed, our audiologists (who have had extensive previous experience in traditional brick and mortar clinics) report a high level of work satisfaction as they get to practice rehabilitative audiology at the height of their license and develop very rich and rewarding relationships with their clients due, in large part, to the additional time they can meaningfully engage with their clients compared to their previous F2F clinical experiences.
With rare exceptions (due to technical issues or challenges with the client’s comfort with the technology), the clinician’s VVV experiences are reported to be at least as effective, and often more so, than their previous F2F encounters. For example, the audiologists often report finding it easier to work with the client and their communication partner since they are often at home together.
Conclusion
The use of telehealth has grown exponentially over the past 4 to 5 months. Clinicians and their clients will require some time to feel fully comfortable with, and learn to navigate, this growing, and currently critical, healthcare delivery innovation.
While it’s true that some people may prefer in-person discussions with their healthcare providers, every day thousands (millions?) of sensitive conversations are successfully conducted via phone or video conference. Perhaps, because the Lively model of hearing healthcare was designed and implemented long before the COVID crisis, our experience and expertise delivering care in a virtual environment have successfully demonstrated that VVVs, when properly conducted by “outstanding audiologists”, are at least as effective as F2F encounters.
References:
- Agha Z, Schapira R, Laud P, McNutt G, Roter D. (2009) Patient satisfaction with physician-patient communication during telemedicine Telemed & e-Health 15(9):830-839
- Donelan K, Barreto E, Sossong S, et al. (2019) Patient and clinician experiences with telehealth for patient follow-up care Am J Manag Care 25(1):40-44
- Eikelboom R, Atlas M. (2005) Attitude to telemedicine, and willingness to use it, in audiology patients. J Telemed & Telecare 11(2): S22-S25
- Gladden C, Beck L, Chandler D. (2015) Tele-audiology: expanding access to hearing care and enhancing patient connectivity. J Am Acad Audiol 26(9):792–799
- Kruse C, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M (2017) Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open 2017;7:e016242. doi:10.1136/bmjopen-2017-016242
 Harvey B. Abrams, Ph.D. is the Head of Research Audiology for Lively. In a 40+ year career, Dr. Abrams has served in a number of academic, clinical, research, and administrative capacities with the Department of Veterans Affairs, the Department of Defense, academia and private industry to include Chief of the Audiology and Speech Pathology Service and Associate Chief of Staff for Research and Development at the Bay Pines VA Healthcare System, the Director of Research at the Army Audiology and Speech Center at Walter Reed Army Medical Center, and the Director of Audiology Research at Starkey Hearing Technologies. He instructs students at several AuD programs and is a frequent lecturer on the topics of outcome measures, health-related quality of life, professional issues, and evidence-based audiologic practice. His research has focused on treatment efficacy and improved quality of life associated with audiologic intervention to include, most recently, computer-based auditory training.
Harvey B. Abrams, Ph.D. is the Head of Research Audiology for Lively. In a 40+ year career, Dr. Abrams has served in a number of academic, clinical, research, and administrative capacities with the Department of Veterans Affairs, the Department of Defense, academia and private industry to include Chief of the Audiology and Speech Pathology Service and Associate Chief of Staff for Research and Development at the Bay Pines VA Healthcare System, the Director of Research at the Army Audiology and Speech Center at Walter Reed Army Medical Center, and the Director of Audiology Research at Starkey Hearing Technologies. He instructs students at several AuD programs and is a frequent lecturer on the topics of outcome measures, health-related quality of life, professional issues, and evidence-based audiologic practice. His research has focused on treatment efficacy and improved quality of life associated with audiologic intervention to include, most recently, computer-based auditory training.







