by Brian Taylor, AuD, Editor-at-Large

Brian Taylor, AuD
If you followed the unveilings at CES 2020, there’s really no doubt hearing aids continue to morph into consumer audio devices, as a growing number of consumer audio devices transform into hearing aids. Obviously, a greater number of choices, spread across a wide range of price points, is a positive development for consumers with hearing loss, especially for millions of people with hearing challenges who don’t want or value interventions delivered by licensed professionals – something covered in Part 1.
The convergence of hearing aid and consumer audio technology is one facet in the continued evolution of the traditionally paternalistic model of healthcare toward interactive, consumer-oriented healthcare. This advancement in heathcare will enable more people to opt to self-direct their own care — the ability to self-assess, self-diagnose, self-treat and self-manage one’s own condition with little to no direct involvement with a licensed professional.
There are two concepts driving this movement toward self-directed care. At the center of each concept is the smartphone, smartphone-enabled apps and a wireless internet connection, which, together, form a user-friendly self-directed care system.
1) Democratization of Technology
Many of the tests and procedures conducted in the clinic by highly trained staff using sophisticated equipment can be placed in the palm of the consumer’s hand, allowing them, smartphone and machine-learning apps in hand, to self-screen for possible ear disease, self-test their hearing or even self-fit hearing aids. These are all part of a larger movement aimed at democratizing all of healthcare. Even if a patient chooses to make an appointment for a comprehensive hearing assessment, the standard test battery can be completed by a non-audiologist using automated equipment. If you’re an aging Baby-boomer or Gen Xer who’s grown up experiencing the marvels of both modern medicine and Madison Avenue marketing, there’s a good chance you find this new found ability to self-direct your own health care incredibly appealing.
2) Decoupling of the Buying Process
Until recently, if you have a hearing loss and decided to pursue hearing aids, the entire sales and service acquistion process took place in a linear manner, as outlined in Figure 1. Vinaya Manchaiah and I wrote in detail about it here. All aspects of the buying process typically occurred with the same clinic, under the same roof. In a sense, persons with hearing loss were hostage to the location in which they decided to do business. The costs of switching to a new provider meant developing new personal relationships with new service providers. An often time consuming and stressful process.
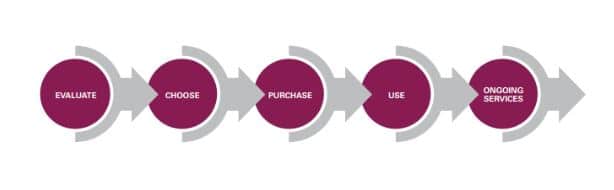
Figure 1. The traditional linear buying process with five key phases, delivered by the same clinic
Now, thanks to modern technology, each phase of the buying process can be delivered by a different clinic or service provider and each of the five phases of the buying process, importantly, can be delivered either face-to-face or virtually, using webcasting, video chatting or some other form of computer-based communication.
Figure 2 and Figure 3 show two examples of a decoupled buying process, in which the consumer with hearing challenges acquires a different component of the buying process from three different entities.
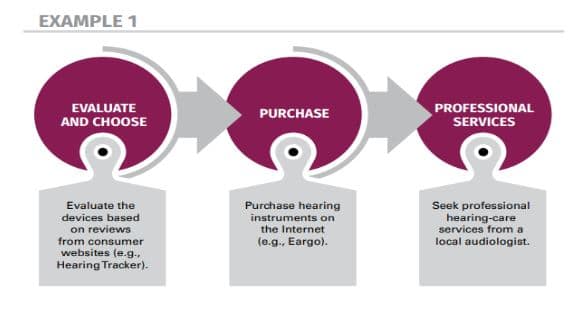
Figure 2. An example of the decoupled hearing aid buying process
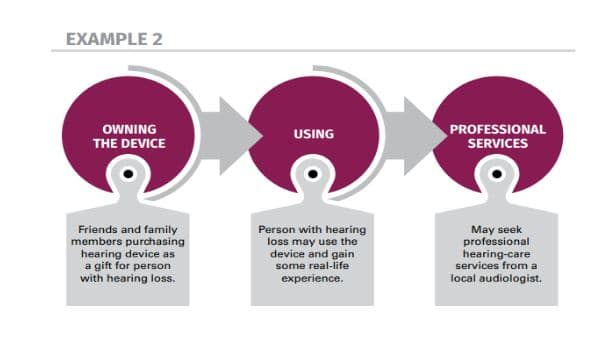
Figure 3. Another example of the decoupled buying process
Given the nature of hearing loss that’s gradual in onset, its accompanying social stigma and the natural inclination to procrastinate intervention for a chronic condition, both the democratization of technology and the decoupling of the buying process enable consumers with hearing challenges to dabble, test drive and experiment with various assessment tools and treatment options in a low-risk manner from the comforts of home or with the help of family and friends.
The democratization of technology combined with the decoupling of the buying process means consumers can choose when and what parts of the buying process they want customized by an expert professional. And, in contrast, they can decide when and what aspects of the buying process they want standardized/automated. You can think of the choice between customization and standardization/automation as one that lies on a continuum, like the one shown in Figure 4.
For every component of the buying process, from evaluation to on-going service (See Figure 1) the consumer with hearing challenges can decide if it’s worth the time and money to have all or some aspect of the buying process customized. Customization, it would seem, of all or some part of the buying process more likely leads to an optimal outcome.
On the other hand, an automated or standardized one-size-fits-all process, which saves either time or money, more likely leads to an outcome that might be “just good enough.”
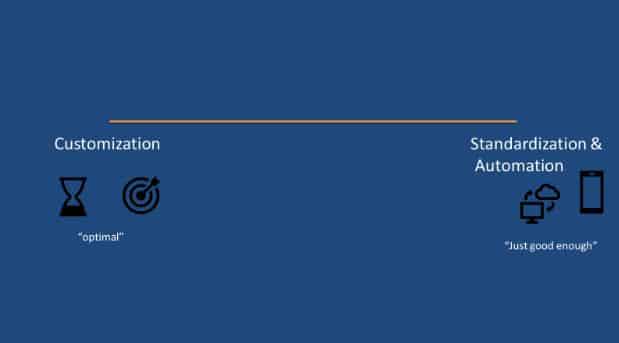
Figure 4. The Customization-Standardization/Automation Continuum. Customization takes more time but it’s more individualized and more often lends to an optimal outcome. Standardization and automation require less time, tend to reduce cost for the patient and more often lead to an outcome “just good enough” for the patient.
Clinicians may soon even practice in a world where customers with hearing challenges begin the process in the clinic with a face-to-face visit and after an initial intake the clinician and consumer mutually decide the rest of the buying process can be automated or standardized with little or no further direct involvement from the professional.
Today, clinicians are already grappling with providing services on this customization – standardization/automation continuum. There are several components of the clinical delivery process that can be standardized or automated, thus saving considerable time, but possibly sacrificing an optimal outcome.
Every clinician uses a standardized procedure to measure hearing thresholds and speech understanding ability – components of a standard assessment that can be completed with automated equipment in the clinic today. And, many clinicians rely on first fit algorithms as a starting point in the fitting process and don’t use probe microphone measures to customize the fitting. Any test, procedure or interaction in the clinic with a patient can be placed somewhere on this continuum.
It seems clear that if hearing care professionals want to remain relevant for most consumers with hearing challenges, they must identify ways to customize as many parts of the buying process as possible.
Further, it makes sense to provide this customization in an a la carte format, allowing consumers the ability to chose what they want customized. Below are some examples of how hearing care professionals can differentiate their practice through customization for each of the stages of the buying process.
Each of the components listed below could be an unbundled fee for service:
(1) Evaluate: Customize Information Gathering and Treatment Goals
Gather as much information as you can about the person’s auditory system and the underlying non-audiological factors that contribute to their handicapping condition. Use scaling questions to gauge the patient’s perception of hearing loss and their willingness to take action on a treatment.
In addition to standardized tests like the Quick SIN, use established questionnaires like the Revised Hearing Handicap Inventory Screening to ascertain the patient’s self-reported emotional and social factors affecting communication ability.
Finely tailored information gathering leads to the development of bespoke treatment goals that can be recorded on the COSI or Patient Expectation Worksheet. Gathering detailed information about the person (not just their auditory system) and devising individualized treatment goals cannot be easily replaced by machine-learning algorithms or standardized tools found on an app or website. It’s a humanistic skill provided by conscientious professionals.
(2) Choose: Customize Treatment Options
One of the tenets of patient centered communication is that the consumer with hearing challenges and the service provider are working together to identify treatment goals and options. By using a patient decision aid, like the one shown in Figure 5, clinicians can educate consumers about a full range of options, including options that may be “just good enough.” It is the responsibility of the clinician to educate the consumer about the pros and cons of every potential treatment option, even those that may be sub-optimal.
Effective decision aids show more than device options but can include the option of doing nothing or forgoing the use of a device and trying some type of stand-alone aural rehabilitation or auditory training program. Patient-centered communication means the provider is clearly articulating the pros and cons of each option based on the information gathered during the evaluation.
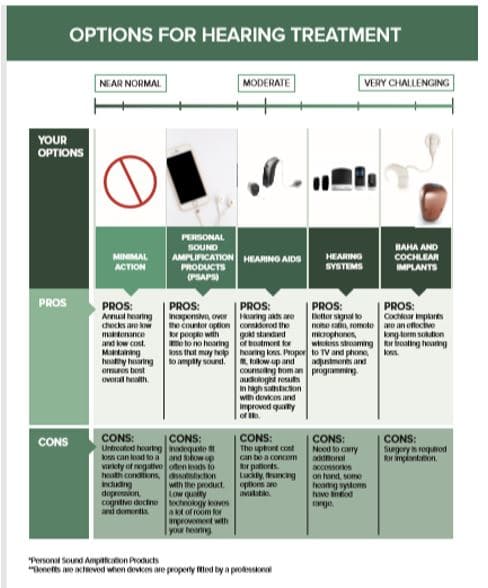
Figure 5. An example of a patient decision aid used to customize treatment options
(3) Purchase: Customize the Fitting
Regardless of where a consumer may have purchased hearing devices, professionals have an opportunity to provide quality control measures to ensure the physical fit and acoustic parameters are optimized.
One proven strategy is to use a scientifically validated prescriptive target and verify the match of that target with probe mic measures. A 2018 study by Valente and colleagues indicates that squeezing an extra 5 to 8 dB out of the fitting, getting the first-fit starting point closer to an individualized prescriptive target, improves speech understanding by upwards of 20%.
The challenge for clinicians, of course, is that they don’t always have familiarity or access to fitting software that allow them to make these necessary adjustments on devices purchased elsewhere. A challenge that could be addressed by changes in FTC hearing aid regulations.
(4) Use and Ongoing Service: Customize Self-Management Plans
More than simply teaching patients how to use their hearing aids, clinicians can customize an individual’s self-management plan. People with chronic conditions, like hearing loss, benefit from learning how to be independent communicators and problem-solvers.
Since their condition cannot be cured but it can be effectively managed, the goal of the professional is to devise a self-management plan, targeting key areas of improvement for the individual. A self-management plan focuses on improving one of the three components of self-management:
- Knowledge of the condition and treatment options,
- Actions that improve the patient’s condition,
- Psycho-social issues resulting from the hearing loss that need to be overcome or addressed through long range planning and support from a professional.
An individualized self-management plan is an iterative process, which means that it is likely to change over time. Therefore, at least once a year the consumer and provider sit down together and update the plan by modified goals and communication strategies.
These are four examples of how hearing care professionals, relying on patient centered communication skills, can customize any link of the buying process for individuals who have the choice of self-directing their care. As a larger number of routine clinical tests, procedures and products become automated and democratized, it is imperative for hearing care professionals of all stripes to excel at the humanistic ability to tailor all components on the buying process in an a la carte manner.
Customizing the consumer’s purchasing experience can be the antidote to automation.
Brian Taylor, AuD, is the director of scientific and product marketing for Sivantos. He is a veteran of the hearing industry with more than 25 years of experience, most recently at Fuel Medical Group where he served as Director of Clinical Audiology. An Audiologist since 1991, Brian received his Au.D. from Central Michigan University in 2006. During his career, Brian has been involved in many areas of the industry including clinical practice, practice and professional development, and training. Brian is a prolific and respected contributor to the industry with more than 25 publications and numerous speaking engagements both domestically and internationally. He has written and edited six textbooks, and most recently authored Essential Business Principles and Tactics for Clinical Managers: The First (or Next) 100 Days. Brian served as Editor-In-Chief at HHTM from 2018-2019 and currently serves as Editor-at-Large.







I am an audiologist who has been in practice for 40 years and current own an independent audiology practice in Ann Arbor, MI. While I certainly agree the “democratization of health care” is a growing trend and one that will not likely fade in the near term, I believe “baby boomers” (of which I am one) and “Gen X” patients have a primary motivation to find the least expensive and most convenient path to whatever they are purchasing. That, of course, is the point of unbundling. What most proponents seem to ignore is that if the overall cost is reduced, that comes from somewhere. The end user is saving, I haven’t seen any reduction in the whole cost of aids to my office, so the savings are coming from the audiologist/dispenser. Salaries, rent etc are not less expensive. I find it unlikely your e “customization” options will find a willing buyer if, in fact, the initial goal was to save money.
Combine that with the influx of 3rd party payers, OTC aids and the specter of Medicare coverage for hearing aids, I fear the independent practice may be an unsupportable relic.