In my last blog post, I reviewed the new GRACE 3 guideline for acute dizziness and vertigo in the emergency department. The first recommendation from that guideline was that Emergency Department (ED) physicians need training in bedside tests such as the HINTS protocol, the Dix-Hallpike test, and performing the Epley maneuver when applicable. I also suggested that those of us in vestibular management should reach out to our ED colleagues and offer training programs, which I did.
 Our ED resident training program graciously put me on the roster for their next grand rounds, which took place last week. Coincidentally and serendipitously, a scheduled talk for earlier that same day was “Identification of Stroke and TIA” with a focus on posterior fossa stroke. The presenter of that talk and I exchanged some notes prior, which allowed me to focus more on how to do the bedside tests (as opposed to why).
Our ED resident training program graciously put me on the roster for their next grand rounds, which took place last week. Coincidentally and serendipitously, a scheduled talk for earlier that same day was “Identification of Stroke and TIA” with a focus on posterior fossa stroke. The presenter of that talk and I exchanged some notes prior, which allowed me to focus more on how to do the bedside tests (as opposed to why).
The audience (mostly ED residents, but also several experienced faculty) was attentive and asked some great questions:
“When patients are acutely vertiginous, will they let you do a head impulse test?”
“Say I do an Epley. What is the follow up to determine if it was successful? What if they are still symptomatic?”
These are great questions not addressed in the guideline.
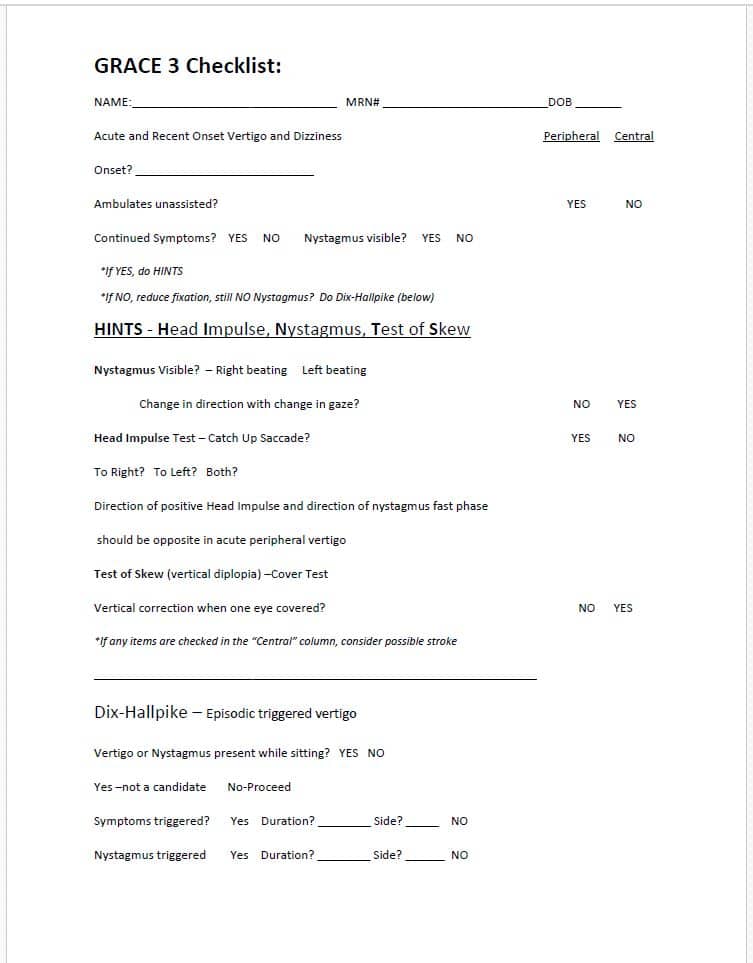
Attempting to identify peripheral vestibular disorders prior to imaging is a paradigm shift for many ED physicians. In order to help guide them through the process, I developed a one page “cheat sheet” for them until they get comfortable with the process. This checklist has not been validated or even used to evaluate its’ efficiency, but it is a start.
Click the image below to access and download the PDF cheat sheet