Editor’s Note: This blog was written by Carrie Nuss, BS. Carrie is a fourth -year AuD student at the University of Louisville, doing a vestibular (among other things) residency at Atrium Wake Forest Medical Center. –Alan Desmond, AuD
by Carrie Nuss
BPPV is common, bothersome, potentially disabling, but generally quickly resolved once a specific diagnosis has been established. The gold standard test for the diagnosis of BPPV is a positive Dix-Hallpike exam, but under the best conditions, sensitivity of Dix-Hallpike testing for active BPPV is less than 100%.
In addition, not all clinics are equipped to perform Dix-Hallpike testing, and not all patients are suitable candidates for provocative testing which involves neck extension. Subsequently, there are a variety of alternative techniques or modifications of the standard Dix-Hallpike test.
This paper reviews some of these techniques.
The Abbreviated Posterior Canalithiasis Chair Based Assessment Maneuver
Posterior canal canalithiasis BPPV is the most common variant of BPPV accounting for 80-95% of all cases (Michael, P., et. al., 2016). The Abbreviated Posterior Canalithiasis Chair Based Assessment Maneuver (APCCAM) aims to diagnose this variant. It is similar to the standard Dix-Hallpike maneuver; however, it requires less specialized equipment.

Image courtesy of Frontiers in Neurology
Since some exam rooms do not have an examination bed or table equipped to do traditional positional testing, the abbreviated maneuver is a useful tool that can be done using a simple backed chair. The patient is asked to begin sitting on the front edge of the chair with their head turned 45 degrees toward the side being tested. They will then be pulled back to the resting position against the back of the chair. Then their head is pulled back into a head hanging position while maintaining the head turn position. This final step is responsible for inducing the movement of the dislodged otoconia, similar to that of laying the patient back flat in the Dix-Hallpike.
When triggered nystagmus and subjective vertigo are considered to the diagnostic criteria, the abbreviated maneuver demonstrated a sensitivity of 80% and a specificity of 96% (Michael, P., et. al., 2016). As described, the APCCAM is very similar to the traditional DHP, however it can be more readily available for use in a wide range of clinics that do not have specialty equipment.
The Loaded Dix-Hallpike Maneuver
The traditional Dix Hallpike test requires the patient’s head to be hanging approximately 30 degrees over the end of the table. Most exam tables do not have the capability to tilt far enough to accomplish this and many patients are unable to lean off the end of the table as needed.
The loaded Dix-Hallpike allows for displacement of particles in a way that does not necessarily require a head hanging maneuver. Jeff Walter, PT, DPT, NCS, proposes that the purpose of the loaded Dix Hallpike is to ensure a higher rate of responsiveness of nystagmus and to reduce false negatives in testing. The loaded Dix-Hallpike requires the head to turn toward the affected side, lean forward with the patient’s nose to the ground while in the sitting position, holding this position for at least 30 seconds before laying the patient flat on their back.
The mechanism behind this maneuver is to “charge up” or “load” the otoconia toward the cupula prior to displacing them within the posterior canal and migrating them away from the cupula.
Loading the otoconia toward the cupula allows them to settle along the cupula, and then the otoconia have a longer period of time to move at their maximum rate through a longer distance in the canal. Additionally, since the otoconia is displaced over a longer timeframe, the clinician is able to observe the nystagmus for a longer period of time ensuring an accurate diagnosis. Although this test has proven to be effective in diagnosing BPPV, there are some drawbacks to completing this test.
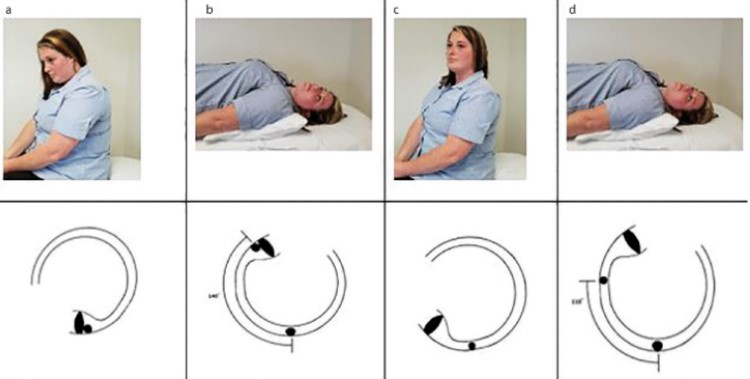
Image courtesy of www.semanticsholar.org
Some patients reported a greater severity of subjective dizziness due to the prolonged movement of the otoconia over a greater distance. There is also the concern of added time that it takes to hold the initial “loaded” position. Despite greater subjective dizziness and potential for longer test times, the Loaded Dix-Hallpike can allow for even less severe BPPV to be detected.
The Mechanical Rotation Chair
Not only is patient mobility a contributing factor to a clinician’s ability to complete a comprehensive test battery for BPPV, but the clinician’s ability to accurately and precisely maneuver the patient can have a significant impact as well. The Mechanical Rotation Chair (MRC) allows for precise, consistent, and accurate movements of a patient during testing that are not always possible with solely an examination bed, table, or chair.
In order for the Dix-Hallpike test to be accurate, the patient must extend their neck 30 degrees below the table. The mechanical rotation chair can accomplish this movement without the additional exertion of extending one’s neck. The MCR can accomplish 360 degrees of movement, while maintaining stability and reducing pressure on the patient’s head and neck. One study conducted by Bech, M. W., et., al., 2023 determined that the MRC was assumed to be the most sensitive test modality and was coined the “gold standard” in sensitivity calculations. The MRC was found to have a sensitivity of 93.9%. An additional convenience of the MRC is that it can also be used for repositioning maneuvers for treatment of BPPV, which can often be difficult to complete on a traditional exam table.

MRC chair. Image credit: Interacoustics
Although the MRC has a high sensitivity rate of accurately diagnosing BPPV, the cost of the machine is significantly higher than any of the other testing modalities.
The Side Lying Test
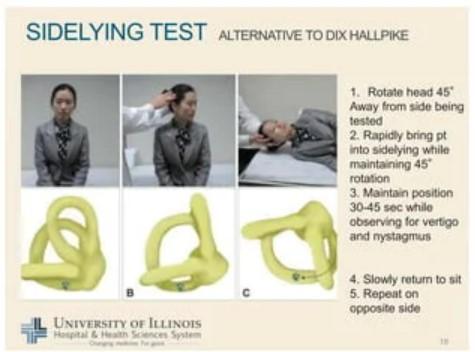
Image courtesy of University of Illinois
As previously discussed, many patients have limited mobility that can hinder a provider’s ability to perform adequate testing. Alternate testing such as the side-lying test, stimulates the posterior semicircular canal by using different movements of the head.
Instead of the traditional movement of the Dix-Hallpike, where the patient’s head is turned toward the side being tested, the side-lying maneuver requires the head to be turned away from the side being tested. In this position, the posterior canal is tested along the frontal plane, rather than the sagittal plane as it is in the Dix-Hallpike. The patient begins sitting on the exam table, they then turn their head 45 degrees away from the side being tested. The patient is then rapidly brought into the side lying position while maintaining head rotation. This position is held for 30 seconds before returning to the seated position.
In a study by Cohen H. S., 2004 that compared the outcomes of diagnosis of posterior canal BPPV from the Dix-Hallpike and the Side-lying maneuver, evidence suggested that there is no significant difference in generation of nystagmus between the two tests. This allows the clinician to utilize the patient’s neck mobility in a way that can stimulate the effected side as needed.
Dix-Hallpike Alternatives for BPPV Diagnosis
Although the Dix-Hallpike is the most widely utilized test to diagnose BPPV, there are effective alternatives that can be modified to a patient or clinician’s needs. The clinician should consider their patient’s mobility as well as their access to equipment when determining the method that will be most useful.
References:
- Bech, M. W., Staffe, A. T., & Hougaard, D. D. (2023). A mechanical rotation chair provides superior diagnostics of benign paroxysmal positional vertigo. Frontiers in neurology, 14, 1040701. https://doi.org/10.3389/fneur.2023.1040701
- Cohen H. S. (2004). Side-lying as an alternative to the Dix-Hallpike test of the posterior canal. Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, 25(2), 130–134. https://doi.org/10.1097/00129492-200403000-00008
- Jeff Walter, P. (2021, September 13). The loaded dix-hallpike: An update in BPPV testing. Medbridge Blog. https://www.medbridge.com/blog/2021/09/the-loaded-dix-hallpike-an-update-in-bppv-testing/
- Michael, P., Oliva, C. E., Nuñez, M., Barraza, C., Faúndez, J. P., & Breinbauer, H. A. (2016). An Abbreviated Diagnostic Maneuver for Posterior Benign Positional Paroxysmal Vertigo. Frontiers in neurology, 7, 115. https://doi.org/10.3389/fneur.2016.00115






