The most common peripheral vestibular disorder is the condition of Benign Paroxysmal Positional Vertigo (BPPV), accounting for anywhere from 17-42% of all patients seen with symptoms of vertigo.1 The condition of BPPV causes brief episodes of vertigo provoked by a head movement or position change.
Benign Paroxysmal Positional Vertigo (BPPV) is typically described by location and type. For example, the most common form of BPPV is posterior canal Canalithiasis.
“Posterior” refers to the location (one can also have BPPV in the Horizontal or Anterior Canal), and Canalithiasis refers to the condition of the otoconia (Are they moving freely or stuck on the cupula?)
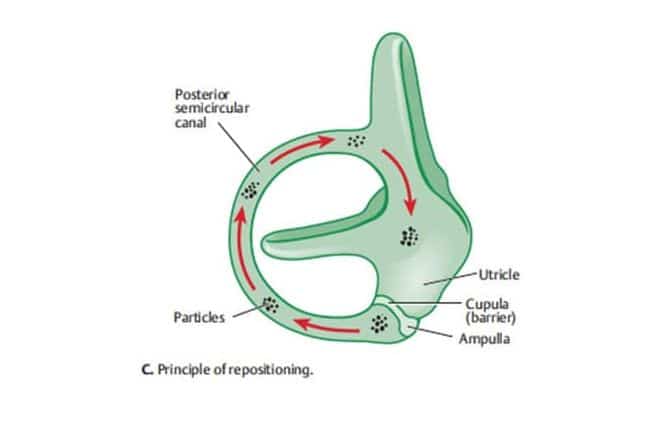
The accumulation of particles in the dependent part of the canal leads to a shift in position, creating a deflection of the cupula. This results in vertigo and torsional nystagmus. The nystagmus is temporary and reverses when the patient returns to an upright position. The response weakens over time as the particles disperse along the canal.
BPPV Diagnosis: Canalithiasis or Cupulolithiasis
In 1969, Dr. Harold Schuknecht first proposed the theory of Cupulolithiasis in which he suggested that BPPV was the result of otoconial debris attached to the cupula of the offending posterior semicircular canal.2 Epley (1992) offered an alternative theory of Canalithiasis, which more thoroughly explains the source of the typical signs and symptoms of BPPV.3
The theory of Canalithiasis proposes that there are free-floating particles (otoconia) that have gravitated from the utricle and collect near the cupula of the posterior canal. When the head is moved into a position that causes the particles to move away from the cupula, the resulting hydrodynamic drag causes cupular deflection (and asymmetric stimulation) resulting in vertigo and nystagmus until the particles come to rest in the now gravitationally dependent section of the canal.
It is likely that both of these conditions exist and treatments have been proposed for both.
Bow and Lean Test
The Bow and Lean Test is one method used to differentiate between Canalithiasis and Cupulolithiasis. By applying Ewald’s Second Law, it helps determine which ear is affected and guides the appropriate treatment. In essence, when fluid flow or otoconia movement in the horizontal canal is directed towards the cupula, it triggers an excitatory response. Conversely, when the cupula deflects away from the utricle and towards the canal, it leads to an inhibitory response. The direction of nystagmus (involuntary eye movement) serves as a crucial indicator, with nystagmus beating toward the more neurally active ear, which is considered excited in this context. This test aids in pinpointing the specific ear requiring treatment for BPPV.
Below readers will find a clip demonstrating the Bow and Lean Test with a patient who presents with Right Horizontal Canal BPPV, Cupulolithiasis-Type
References:
- Battacharyya, N., Gubbels, S.P., Schwartz, S.R., Edlow, J.A., El-Kashlan, H., Fife, T. ……& Corrigan, M.D. (2017) Clinical practice guideline: Benign paroxysmal positional vertigo (update). Otolaryngology-Head and Neck Surgery. 156(3S): S1-S47.
- Schuknecht, H. F. (1969). Cupulolithiasis. Arch Otolaryngol Head Neck Surg, 90, 765–778
- Epley, J. (1992). The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg, 107(3), 399–404
 Alan Desmond, AuD, is the director of the Balance Disorders Program at Wake Forest Baptist Health Center, and holds an adjunct assistant professor faculty position at the Wake Forest School of Medicine. He has written several books and book chapters on balance disorders and vestibular function. He is the co-author of the Clinical Practice Guideline for Benign Paroxysmal Positional Vertigo (BPPV). In 2015, he was the recipient of the President’s Award from the American Academy of Audiology.
Alan Desmond, AuD, is the director of the Balance Disorders Program at Wake Forest Baptist Health Center, and holds an adjunct assistant professor faculty position at the Wake Forest School of Medicine. He has written several books and book chapters on balance disorders and vestibular function. He is the co-author of the Clinical Practice Guideline for Benign Paroxysmal Positional Vertigo (BPPV). In 2015, he was the recipient of the President’s Award from the American Academy of Audiology.
**this piece has been updated for clarity. It originally published on May 14, 2013







Is it possible to have BPPV without nystagmus? I have been suffering with constant vertigo for around six years now and am at my wits end. Despite seeing 4 different ENT’s and 3 neurologists, no cause has been identified. I have been thoroughly observed for nystagmus, and do not have tinnitus. It certainly can be positional, but even with the slightest movements of the head or eyes.
It is possible that you could have BPPV and it not be present at the time of examination. If the physicians did the Dix-Hallpike test where they lay you down quickly with your head to the side, did it trigger your symptoms? If so, nystagmus should be present if, in fact, you have BPPV. But, if they did not trigger any vertigo, they would not see any nystagmus associated with BPPV.
Your description of “constant vertigo” is inconsistent with BPPV. BPPV typically causes short episodes (less than one minute) of acute vertigo, brought on by head movement such as lying down or rolling over in bed.
My husband has been diagnosed with Positional Vertigo-posterior canal cupulolithiasis. The dizziness and unsteadiness is making him feel very uncomfortable. He has been prescribed tab, Stugeron 25mg twice daily and tab. Stemetil MD 5mg. twice daily. He has been taking it for the last three days but finds little change. He has been on medicines for blood pressure which is in normal range. Could you let me know if the line of treatment is correct and how long will it be before he is able to feel comfortable again. He is 53 years old. Thankyou.
I am not a medical doctor, so it would be out of my scope of practice to make suggestions regarding medications.
I recently had a VNG which included Oculomotor Study, Active Head Rotation, Positional Tests, Dix/Hallpike Test, and Caloric Tests. The Impressions of the Physician indicate evidence of significant peripheral and central dysfunction suggestive of benign paroxysmal positional vertigo in addition to other apparent issues. The Physicians recommendation is Balance rehabilitation and Canalith repositioning (e.g. Epley) maneuvers.
What does all this mean???
Paul:
It would be impossible for me to accurately unwind all this for you. The statement “evidence of significant peripheral and central dysfunction suggestive of benign paroxysmal positional vertigo ” concerns me because BPPV is not associated with central vestibular dysfunction. I would suggest that you make sure you are seeing a neurologist, otolaryngologist or audiologist that specializes in vestibular disorders.
Contact Newport Mesa Audiology Balance and Ear institute for a confident evaluation of your vestibular system. My mother went to this facility and had success with their expertise and state of the art equipment. She participated in 6 weeks of vestibular therapy and no longer has any symptoms. She did not have BPPV, but they can treat BPPV at the same time as diagnosing, if they do in fact diagnose it. All 10 of the audiologists are great.
I have been diagnosed with cupulolithiasis and now my other ear is affected. I am wondering how is it possible to have 2 “rare” conditions at the same time … cupulolithiasis and bilateral BPPV? Tried Epley and Semont maneuvers and nothing works. Going on 2 months now. No one seems to know how to help me. Any ideas?
Forgot to add … both are in the posterior canals.