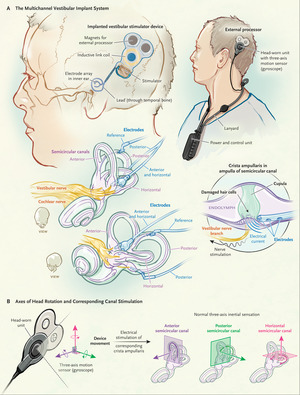
Components and Mechanism of a Vestibular Implant. Image credit: NEJM
The vestibular system has two primary roles: to provide visual stability during head movements and to assist with postural control. The peripheral (inner ear) vestibular system is able to do this with three semicircular canals (angular sensors) and two otolith organs (linear sensors) on each side. The information coded by these organs is transmitted to the brain and either sent to the eyes for reflexive eye movement through the vestibular ocular reflex or to the lower extremities for postural control through the vestibular spinal reflex.
Dysfunction of this system can lead to dizziness, imbalance, and nausea.
Currently peripheral vestibular disorders are managed through physical therapy often referred to as vestibular rehabilitation. Vestibular rehabilitation can assist in a process called compensation where the brain re-calibrates vestibular information to best provide visual stability and assist with postural control in cases of unilateral peripheral vestibular (inner ear) dysfunction. For compensation to occur, there must be at least some function in one of the inner ears. It is important to note that even a well-compensated vestibular injury doesn’t mean complete lack of symptoms as the vestibular system is all that allows for visual stability with rapid head movement.
Vestibular rehabilitation is also currently the only available way to manage a bilateral peripheral vestibular weakness or loss of function. In this case, the aim is not to compensate for the injury, but rather to substitute information from the senses of vision and touch to allow for some degree of postural and visual stability while moving.
Many individuals with bilateral loss of peripheral vestibular function suffer from debilitating dizziness, bouncing vision (oscillopsia) when they move their head, and severe imbalance. Individuals with bilateral weakness are much more likely to fall, suffer from a large disease related economic burden, experience activity limitations, and social withdrawal due to the symptoms. The management strategies are currently limited with inner ear disorders and the outcomes from those with bilateral vestibular weakness are particularly poor.
What is a Vestibular Implant?
In recent years, there has been research into treating patients with bilateral vestibular loss of function with a vestibular implant. This device codes head movement with an external processor and converts the head movement into an electrical current that stimulates the corresponding inner ear organ based on the direction of head movement.
Cochlear implants have been used similarly by converting acoustic energy into an electrical current that stimulates the hearing nerve for many years with good outcomes.
Current Evidence for Vestibular Implantation
There are currently very few patients utilizing vestibular implants and the long-term outcomes with these devices are largely unknown.
A recent NIH funded study “Posture, Gait, Quality of Life, and Hearing with a Vestibular Implant” examined the outcomes of 7 participants that received vestibular implants at 6 months and 12 months after implantation with promising results.
Objective Measures
Measures of standing balance included the modified Romberg and the balance subtest 5 of the Bruininks-Oseretsky Test of Motor Proficiency. At follow-up, the Romberg scores more than doubled, indicating participants were able to stand on a foam surface with their eyes closed for twice as long compared to pre-implantation.
The Bruininks-Oseretsky Test scores improved significantly as well, indicating better balance when standing on one foot, standing on a balance beam, and standing heel to toe compared to pre-implantation scores.
Measures of gait performance included the Dynamic Gait Index and the Timed Up and Go. The Dynamic Gait Index scores improved significantly showing better performance while walking with head movements and stepping around obstacles. The Timed Up and Go scores revealed significantly increased gait speeds.
Subjective Measures
Measures of self-perceived dizziness handicap, quality of life and the effect on one’s activities of daily living were assessed with the Dizziness Handicap Inventory, Vestibular Disorders Activities of Daily Living questionnaire, and the Short Form Health Survey. The Dizziness Handicap Inventory average score went from a severe perceived handicap pre-implantation to a mild handicap following implantation at 6 and 12 months.
There was also a significant improvement in participants’ abilities to perform their activities of daily living and self-rated improved quality of life.
Outcomes
All objective measures of standing balance and gait showed a significant improvement at both 6 month and 12 month follow up post vestibular implantation. All participants rated that the vestibular implant improved their quality of life, improved their abilities to perform their daily activities, and reduced their perceived handicap from their dizziness.
All patients exhibited some decrease in hearing in the ear that was implanted. This decrease in hearing was mild for most participants, but 37% of those that received the vestibular implant experienced a severe to profound hearing loss in the implanted ear. The authors speculated that changes in future surgical techniques may reduce the risk of significant permanent hearing loss associated with the procedure.
Vestibular implantation has been shown to significantly improve balance and reduce the handicap associated with bilateral vestibular loss of function. Previously, this was a patient population with limited treatment options and vestibular implantation could potentially provide these patients with a better quality of life and reduce their risk of falls. This procedure does not appear to be without risk and can cause hearing loss in some individuals. This was a small-scale study and larger scale studies would be helpful to better determine all of the potential benefits and risks of vestibular implantation.
Nevertheless, these are promising findings for a treatment option for those with bilateral loss of peripheral vestibular function.
Readers may also be interested in the video below from Johns Hopkins:








Your article was so smart and also inspiring. I am extremely interested in receiving an implant. I have a 13 year old debilitating case of Bilateral Vestibulopathy, and as you so importantly point out, VRT does not work for us. If you have any info on purchasing the implant or getting on a clinical trial list, I would be so grateful. I live in NYC, but I will go wherever necessary.
Thank you so much for this important well written article,
Kay Brover
Your article was so smart and also inspiring. I am extremely interested in receiving an implant. I have a 13 year old debilitating case of Bilateral Vestibulopathy, and as you so importantly point out, VRT does not work for us. If you have any info on purchasing the implant or getting on a clinical trial list, I would be so grateful. I live in NYC, but I will go wherever necessary.
Thank you so much for this important well written arti
Kay,
I am glad that you found the blog to be helpful. Unfortunately I don’t have any special insight into how you could become a part of this research. If you could get in contact with one of the investigators on this study I am sure they could guide you better.
Best,
Brady Workman
I incurred walking difficulty in 2005. I did not secure a correct diagnoses until March 2017 at JFK Hospital in Edison, New Jersey, which was
Bilateral Vestibular Loss. Two previous diagnoses were Mild Parkinson and C.I.D.P. It took 12 years to find a doctor able to identify my
Vestibular condition. Many physical therapy sessions all to no avail. I, too, am aware of the multichannel Vestibular trials being held at
Johns Hopkins Medical Center. Hopefully a multichannel device will be forthcoming soon. I volunteered for the Johns Hopkins Vestibular
trials in 2018 or 2019, but was not accepted. I still search for a Vestibular research in New Jersey that I might volunteer for……..
I now use a Veterans Administration electric scooter for doctor visits……
Hi John,
I just discovered your comment this morning, and I have never, in all my debilitating years, talked to anyone else in my proximate condition. Would you be interested in comparing notes, drs., therapies, etc.????