This article discusses the Audiology Crisis and the GSI AMTAS as one potential solution through questions answered by Tony Lombardo, Clinical Application Specialist, and Laura Prigge, Manager of Clinical Education and Training at Grason-Stadler.
Q1: What is the audiology crisis, and what are its primary causes?
Prigge: The audiology crisis refers to the growing gap between the increasing demand for hearing healthcare services and the number of audiologists available to provide care. Despite the aging population and the rising need for hearing health services, the number of audiologists entering the field has not kept pace.
In 2009, a study by Windmill and Freeman found that the number of new audiologists in the U.S. needed to increase by 50% immediately to meet this demand. However, since then, the profession has remained stagnant. This shortage isn’t limited to the U.S.; it’s a global issue.
Many practices are overwhelmed, with some reporting wait times of several months just to schedule a basic hearing test. While awareness of the issue has grown, many practitioners may not realize the full extent of the crisis until they experience these scheduling backlogs or patient overload firsthand.
Q2: How is the audiology crisis impacting patient care?
Prigge: The crisis is having a significant negative impact on patients across various demographics. There is a growing backlog, with many patients facing long wait times to secure an appointment for even a basic hearing test. This issue isn’t limited to older adults; it also affects pediatric patients, school-age children, and adults of all ages with hearing issues.
Lombardo: Also, access to care is even more limited in rural areas. Most audiologists are concentrated in high-population centers, leaving rural communities underserved. This geographical imbalance compounds the problem, making it difficult for patients in less populated areas to access the hearing care they need.
Q3: What are the potential solutions to the audiology crisis?
Prigge: The first part of the solution to the crisis in audiology is to either increase the number of audiologists or increase access to hearing healthcare.
Lombardo: Concurrently, it is our responsibility as hearing healthcare professionals to increase awareness with the overall goal of preventing noise induced hearing loss.
Prigge: Hearing healthcare professionals have dabbled in teleaudiology; however, to address this increasing gap, it’s important to reconsider the methods of teleaudiology and their benefits. There are two approaches to teleaudiology.
Synchronous or live video teleaudiology involves real-time communication between the audiologist and the patient via video. A technician on-site assists with tasks such as placing transducers or conducting video otoscopy, while the audiologist controls the software remotely. This method helps overcome geographic barriers.
Asynchronous or store-and-forward teleaudiology involves test methods that are done independently or with the assistance of a telehealth technician. The results are stored and then forwarded to an audiologist for interpretation. These Store and Forward tests can include video otoscopy, middle ear analysis, and basic diagnostic audiometry. This method overcomes both geographical and time barriers because the audiologist does not have to be present for the procedures.
Both types are valuable for practices considering teleaudiology. AMTAS functions as an asynchronous assessment tool that helps alleviate the audiology crisis while easing the daily workload for audiologists.
Q4: What is AMTAS?
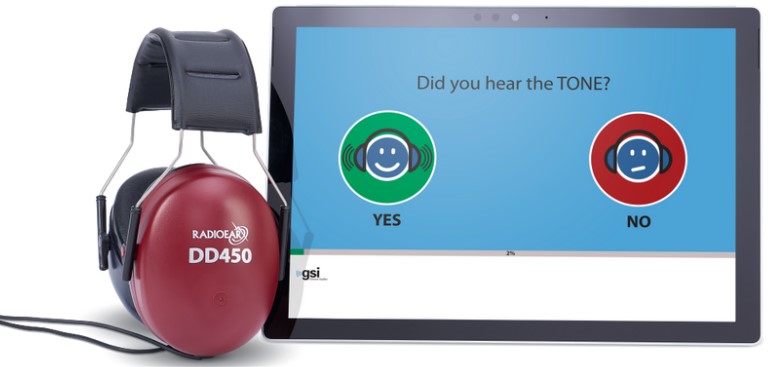
Lombardo: AMTAS (Automated Method for Testing Auditory Sensitivity) is a software tool that allows patients to conduct hearing tests in an automated, self-guided manner. It performs pure tone air and bone conduction tests with masking, as well as masked speech testing: Speech Reception Threshold and Word Recognition.
When the appointment is completed, the results are forwarded to the audiologist for interpretation. In addition to the audiogram and speech results, the interpreting audiologist reviews the patient’s Quality Indicators. Quality Indicators are a list of behaviors that contribute to the validity and reliability of the test. In other words, the patient behaviors have been quantified and the audiologist can make decisions on appropriate next steps with confidence.

Q5: What are the main benefits of GSI AMTAS?
Prigge: GSI AMTAS provides several key benefits. It increases efficiency by automating assessments, reducing the time audiologists spend on basic evaluations, and enhances accuracy with reliable results for accurate diagnoses.
The tool also improves patient access through remote assessments, particularly in underserved areas, and streamlines workflow by integrating with existing systems to organize patient data effectively.
Additionally, it optimizes resources by allowing audiologists to focus on complex diagnostics and addresses the audiology crisis. Finally, its user-friendly interface ensures quick familiarity for users, contributing to better patient outcomes and a more effective practice.
Q6: How long has AMTAS been available, and how was it developed?
Prigge: AMTAS was developed over 30 years ago by Dr. Robert Margolis. While managing the audiology clinic at the University of Minnesota, he saw how much time audiology students spent on basic pure tone tests, which limited their ability to perform more complex diagnostics. This inspired the development of AMTAS to improve both efficiency and accuracy.
Dr. Margolis partnered with Grason-Stadler and officially launched AMTAS in 2016. Since then, ongoing enhancements have been made with input from Dr. Margolis. There have been many studies over the past several years that continue to prove the validity of the evaluation. While AMTAS was originally developed to help ease the workload of a busy clinic, it has evolved into a tool to increase access to hearing healthcare globally.
Q7: Are there instances where AMTAS may not be suitable?
Prigge: AMTAS, like any audiometric evaluation, should not be used as a standalone tool for critical diagnoses. The cross-check principle still applies, meaning AMTAS should be combined with other tests for a full assessment. However, AMTAS is generally appropriate when used alongside other evaluations.
There are a couple of requirements for successful completion of AMTAS. First, the patient must be able to see the touch screen to respond. Second, if doing speech testing, the patient must be able to read English. Additional things to consider are dexterity, mobility, and cognitive function. Validation studies indicate that patients should not be immediately disqualified due to age.
It’s important to note that while AMTAS provides valuable data, the **audiogram alone** doesn’t tell the full story. A trained hearing healthcare professional must interpret the full report, including the quality indicators, to assess the patient’s performance and reliability during the test. This ensures that the data is accurate and meaningful, just as with manual testing.
Q8: What resources does GSI offer for learning more about AMTAS?
Lombardo: GSI offers several great resources for learning about AMTAS. The YouTube channel features a variety of content, including Q&A sessions, tutorials on how to implement AMTAS, set it up, and prepare patients. There are also guest speakers like Dr. Bob Margolis and Dr. James Hall.
Prigge: Additionally, Audiology Online provides multiple webinars on Teleaudiology and AMTAS, offering deeper insights for those looking to explore these topics further.
To learn more about AMTAS please reach out to your e3 Diagnostics Sales Representative.
e3 Diagnostics is the leading distributor of audiological and balance equipment in the U.S. Visit the main website to view the product offerings, schedule annual equipment calibration, or request service: e3diagnostics.com
Laura Prigge, AuD, is the Manager of Clinical Education and Training with GSI. Laura received her Doctorate of Audiology degree from AT Still University. Laura’s 25+ years of experience includes providing manufacturing support for a leading hearing aid manufacturer as well as technical audiology training and support for an international audiologic equipment company. Prior to that, she managed education and training at another hearing aid manufacturer and conducted audiologic evaluations on children, adults, and geriatric patients at a retail hearing center.
Tony Lombardo, MS is a second-generation audiologist who received his Masters from the University of Wisconsin-Oshkosh with an emphasis on pediatric audiology. He has over 20 years of experience in the hearing industry working in a variety of settings. He has experience performing diagnostic testing with all age ranges, industrial audiology, retail, hearing aid financing and insurance, and industry trade shows. At GSI Tony is focused on training, support and education.