
Brian Taylor, AuD
Any business with more than two employees is likely to have a written set of policies and procedures. You know – that binder hidden under a stack of papers on your desk where these policies and procedures reside, often collecting dust.
Eventually there is a moment – an occasion when your business gets into a jam, an employee has a question or there is some type of legal dispute. When that happens, we lean heavily into those policies and procedures to navigate the problem as smoothly as possible.
Clinical practices, which are, after all, businesses, have policies and procedures that are used to steer a clear path for employees, but those policies and procedures, which might help us clarify questions about sick time or reimbursement for an educational seminar, don’t really help us with patient care. Luckily, about five years ago, a group of concerned clinicians, the Audiology Practice Standards Organization (APSO), decided it was time to create some clinical policies and procedures.
Like your HR department’s policy manual, APSO’s clinical standards are a set of principles that ensure audiologists provide high-quality care. Unlike that HR policy manual, though, clinical standards and principles are applied to every patient encounter. Clinical standards also provide a framework for evaluating care and can be extremely helpful if a legal dispute arises over the quality of care provided to a patient. Importantly, standards, which tell us what to do in certain situations, are not the same as guidelines, which tell us how to do it. And, to be clear, standards are not the same as best practices, which tell us how to achieve optimal results. Although standards, guidelines and best practices represent different facets of clinical practice, they do fit together to form a hierarchy of care like the one illustrated in Figure 1.
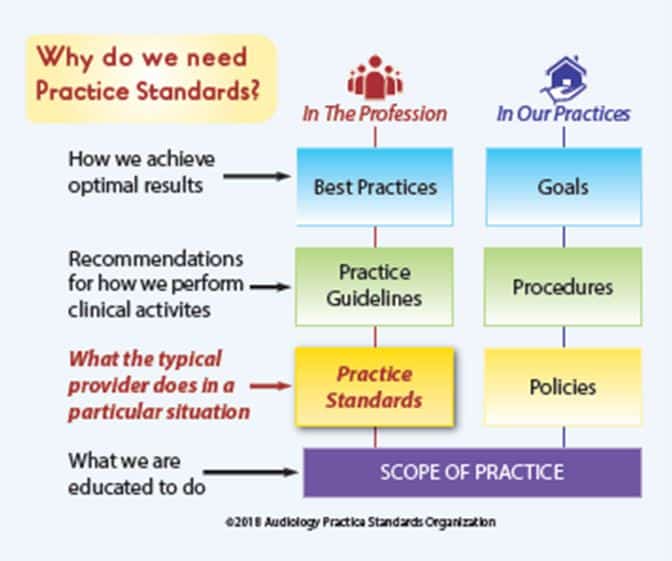
Figure 1. How standards, guidelines and best-practices fit together. Image from Tunnell, J. (2020). 20Q: Why we need an audiology practice standards association. AudiologyOnline, Article 26955. Credit AudiologyOnline
Currently, APSO has published three clinical standards, while at least three more are at some stage of the review process.
You can go to their website to see their progress. Although APSO has been methodically creating practice standards for more than five years, I have observed that few audiologists know they exist. For these reasons, I am posting S2.1 Hearing Aid Fitting for Adult & Geriatric Patients, their 15-item standard for fitting hearing aids.
Hearing Aid Fitting Standard
- The hearing aid selection and fitting process is based on a comprehensive, valid audiological assessment. Each step of the selection and fitting process and the rationale is documented, where appropriate.
- Patient communication is conducted in a clear, empathetic manner consistent with the patient’s communication mode, comprehension, and their health literacy level. Patient-centered and family-centered care is provided. The patient is encouraged to include communication partners (e.g., family members, significant others, companions) throughout the selection, fitting, and follow-up process.
- A needs assessment is conducted in determining candidacy and in making individualized amplification recommendations. A needs assessment includes audiologic, physical, communication, listening, self-assessment, and other pertinent factors affecting patient outcomes.
- Pre-fitting testing includes assessment of speech recognition in noise, unless clinically inappropriate, and frequency-specific loudness discomfort levels. Other validated measures of auditory and non-auditory abilities are considered, as appropriate for the individual patient.
- Fitting of bilateral hearing aids is the recommended protocol if the patient is a candidate for hearing aids in both ears and it is supported by the needs assessment.
- The hearing aid style and the ear coupling are chosen to be appropriate for the degree and configuration of the hearing loss. Style and coupling should reflect any physical limitations of the patient. Patient input regarding acceptable styles is taken into account.
- The recommended hearing aids include signal processing and features that support the patient’s listening needs. They have the appropriate gain and output, including reserve gain, to meet frequency-specific fitting targets as defined by a validated prescriptive method.
- Assistive technology and accessories are considered to facilitate accessibility to other devices and to satisfy the patient’s listening and communication needs.
- An assessment of initial product quality is completed, using standard electroacoustic measures to verify either manufacturer or published specifications.
- Hearing aids are fitted so that various input levels of speech result in verified ear canal output that meets the frequency-specific targets provided by a validated prescriptive method. The frequency-specific maximum power output is adjusted to optimize the patient’s residual dynamic range and ensure that the output does not exceed the patient’s loudness discomfort levels.
- Following individualized verification of hearing aid gain and output, if the fitting is not acceptable to the patient, minor deviations in gain and output may be necessary.
- Orientation is device- and patient-centered and includes use, care, and maintenance of the hearing aid(s) and accessories.
- Counseling is conducted to ensure appropriate adjustment to amplification and to address other concerns regarding communication. Additional rehabilitative audiology is recommended if deemed appropriate.
- Hearing aid outcome measures are conducted. These may include validated self-assessment or communication inventories and aided speech recognition assessment.
- Short- and long-term follow-up is conducted to ensure that post-fitting needs are addressed. This includes updated audiological assessment, hearing aid adjustments and routine maintenance as needed to ensure the devices are functioning properly and appropriately for the patient.

Now for the “How”
As I mentioned earlier, these 15 items tell us what to do, not how to do it. So, if you are a less experienced clinician or one that appreciates a lot of detail, you might find the standards to be lacking specifics (this is not a knock on the standards).
If you want more details on how to conduct or perform each S2.1 standard, Gus Mueller and I created a “Hearing Aid Fitting Toolbox.” It is Volume 6 of our Research Quick Takes series, archived at AudiologyOnline. I think our toolbox serves as the guidelines for many of the S2.1 standards. Our toolbox, which is based on published research, addresses many of these 15-items.
As outlined in Figure 2, there are three recorded (video) courses and two text-based courses. Each course has CEUs attached to it, too.
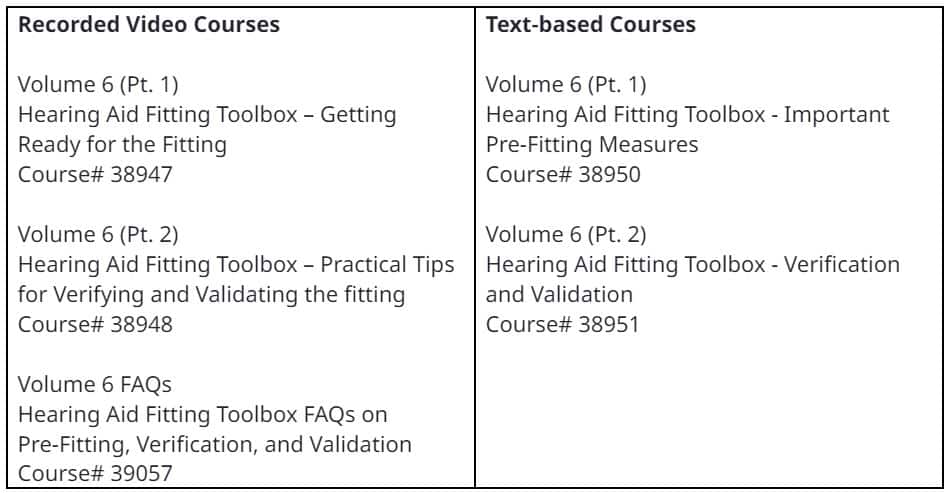
Figure 2. Hearing Aid Fitting Toolbox. Volume 6 of Research Quick Takes
You can access the toolbox, and all the other Research Quick Takes at:
- Research QuickTakes Volume 6 (Pt. 1): Hearing Aid Fitting Toolbox – Important Pre-Fitting Measures
- Research QuickTakes Volume 6: Hearing Aid Fitting Toolbox FAQs on Pre-Fitting, Verification, and Validation
- Research QuickTakes Volume 6 (Pt. 2): Hearing Aid Fitting Toolbox – Verification and Validation
So far, I’ve covered standards and guidelines. You might be wondering where best practices fit into the equation. To better understand where best practices fit in, let me quote an excellent 2020 20Q article from Jenne Tunnell on the topic:
“I like to use a cooking analogy: A cooking standard might state that you should eat healthy foods and prepare foods in a clean and safe environment. Cooking guidelines would detail what are healthy foods, in what proportions they should be consumed, and in what environment they should be prepared. Best practices would indicate that you should use fresh ingredients, instead of preserved ingredients, in order to achieve optimal results.”
In short, best practices are the little things you do in applying the standards and guidelines with each patient encounter. Best practices include the way you say things or the extra time that you take with a certain procedure. It could even be the use of a colorful and easy-to-understand visual aid that educates an older person with hearing loss and cognitive decline. It might be including family members in the assessment and treatment planning process. It’s anything that you might use to personalize each interaction with patients.
As Dr. Tunnell says, best practices are the use of fresh ingredients to achieve the best results. A process that often starts with a trip to the farmer’s market. Let APSO’s standards and the Hearing Aid Fitting Toolbox be your trip to Whole Foods or your favorite farmer’s market.
About the Author
Brian Taylor, AuD, is the senior director of audiology for Signia. He is also the editor of Audiology Practices, a quarterly journal of the Academy of Doctors of Audiology, editor-at-large for Hearing Health and Technology Matters and adjunct instructor at the University of Wisconsin.






