“Signal & Noise” is a bimonthly column by Brian Taylor, AuD.
Part 1 of this post last week took on the the first of three, interconnected, fundamental questions at the core of the evolving marketplace for hearing care services. Each of the three is worthy of deliberation and debate by all hearing care professionals, especially now amidst an abundance of recent noise in the industry and profession.
Deliberation on Q1, “How do we contend with a rapidly aging population that often wants a fundamentally different relationship with a shortage of hearing care professionals?“, concluded with a change directive to audiologists:
Audiologists need to take an active role in the [use of] triaging tools with a goal of maintaining the accurate identification of ear disease, while increasing access to hearing care treatment and management options for a growing aging population.
Q2: How do we leverage the science, which continues to provide evidence of the impact of ARHL on all facets of life, including death, to grow the demand for hearing care services?
Age-related hearing loss (ARHL) has been shown in several well-designed, peer reviewed studies to be associated with myriad negative consequences, including social isolation, depressive symptoms, poor quality of life, reduced independence, lower career earnings and increased risk of mortality. Age-related hearing loss has even been associated with increases in cost of care and hospitalization.
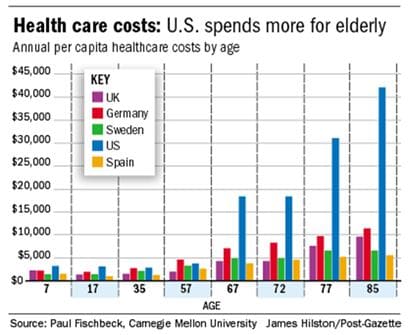
Figure 1. Health care costs associated with age in five countries. Data provided by John Bakke and Bob Tysoe.
These negative consequences associated with ARHL don’t occur in a vacuum. Given the increased healthcare costs associated with growing older, everyone must find ways to make the delivery of healthcare more efficient.
Figure 1 shows the dramatic surge in costs associated with taking care of elderly patients. A relatively high percentage of this high risk, costly population also has ARHL, which likely affects their ability to communicate.
We need to understand the greater cost reductions in healthcare associated with earlier identification and remediation of hearing loss in older adults. Being able to hear and comprehend the physician’s directives during an appointment is important, but we really don’t know how much of an impact hearing loss has on the overall cost of care.
Fortunately, we have leaders in our profession addressing these issues. For example, The University of Pittsburgh Medical Center’s audiology department ,under the direction of Catherine Palmer and Lori Zitelli ,has orchestrated an interventional audiology program, which was written about in the latest issue of Audiology Practices. We need more programs of this type – where audiologists proactively identify and remediate hearing loss while medical care is being delivered.
The relationship between ARHL and other medical conditions requires audiologists to take an active role in the emerging integrated, accountable care organizations around the country. Because the nature of age-related hearing loss is progressive and gradual (and likely less expensive to ameliorate when identified earlier) in the vast majority of individuals, professionals involved in hearing care must intervene sooner when patients are younger and have milder hearing loss.
Q3. How do we bridge the gap between access and innovation?
As evidence mounts that early identification and treatment stave off many of the ill-effects of ARHL, it’s a reasonable assumption that all patients with the condition need access to affordable and effective hearing aid technology. Today, due to a combination of high costs, stigma and a lack of guaranteed success with hearing aids, uptake remains low, especially for younger individuals with milder hearing loss.
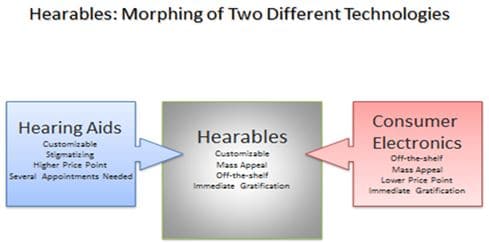
Figure 3. Some of the key attributes of hearing aids and consumer electronics morph to create a new product category called hearables.
Concurrently, technological innovations continue to increase. We are seeing the rise of hearables, which are a morphing of conventional hearing aid technology and consumer electronic devices, as shown in Figure 3. For consumers hearables may offer an appealing option, but current FDA regulations largely preclude their use for individuals with hearing loss.
Hearing aid manufacturers who enjoy large profit margins in a market 25% to 40 % penetrated are unlikely to risk the cannibalization of their existing business by introducing less expensive technology into the marketplace, even in the face of evidence suggesting lower cost technology provides essentially the same performance as technology at a premium price point.
Audiologists must act as change agents for their patients, rather than defend the status quo. We must look for ways to grow the demand for hearing care by offering alternative and complementary products and therapies to a rapidly aging population. This starts by recognizing there are two separate and distinct markets for hearing care services. One market is comprised of the approximate 25% of individuals with moderate to severe, more complex, hearing loss requiring a customizable, higher tech solution. The second market consists of the vast majority of hearing impaired individuals with mild to high frequency moderate losses, who are often younger and perhaps more amenable to “one-size-fits all” gadgetry.
Taken further, there is emerging evidence from one soon-to-be-published study and one review article suggesting that a relatively high percentage of individuals with normal audiograms (and mild hearing loss) have an inability to communicate in common, everyday listening situations. It’s reasonable to surmise these groups would benefit from technology at a lower price point, as milder communication problems warrant a less costly solution.
Focus on the Signal, Ignore the Noise
There have been many recent roadside attractions worthy of scrutiny and attention, but we cannot allow them to divert our attention from the real issues facing our profession. How we address the three questions posed in parts 1 and 2 of this post will determine our professional future and the role we play in creating value for individuals of all ages with communication difficulties.
Brian Taylor, AuD, is Senior Director, Clinical Affairs, for Turtle Beach/Hypersound. He continues to serve as Editor of Audiology Practices, the quarterly publication of the Academy of Doctors of Audiology. During the first fifteen years of his career, he practiced clinical audiology in both medical and retail settings. Since 2005, Dr. Taylor has held a variety of leadership & management positions within the hearing aid industry in both the United States and Europe. He has published over 50 articles and book chapters on topics related to hearing aids, diagnostic audiology and business management. Brian has authored three text books: Fitting and Dispensing Hearing Aids (co-authored with Gus Mueller), Consultative Selling Skills for Audiologists, and Quality in Audiology: Design & Implementation of the Patient Experience. His latest book, Marketing in an Audiology Practice, was published in March, 2015. Brian lives in Golden Valley, MN with his wife and three sons. He can be reached at [email protected] or [email protected].
feature image courtesy of Cambridge in Color






