By Brian Taylor
Last week at Hearing Views, I talked about why so many audiologists and other hearing care providers look out from their offices and see empty waiting rooms. I also discussed some defense strategies that practitioners can deploy to protect our profession from disruptive innovations that threaten its future.
This week, I’m suggesting some offensive strategies that will help audiologists change their business model so that it places service and rehabilitation, rather than a device, at the center of the provider-consumer relationship. By doing this, they will be able to build a business that attracts segments of the market that have not been well served by traditional practice models.
Following are seven ways to differentiate your practice from the competition and to fill your waiting room with more patients. I have divided them into five actions you can take to offer greater value to the segment of the market that most of us are currently serving, and two tactics designed to attract new, untapped segments of the market.
ENHANCE YOUR VALUE TO YOUR CURRENT MARKET SEGMENT
(1) Make your clinic a destination
Find a theme and a few signature moments that have emotional appeal to patients. The traditional medical practice’s waiting room is mundane and sterile. To take that thought further, the entire patient experience with just about any type of medical practice is ordinary at best. There is no reason for healthcare professionals to ignore what every other industry has been doing for years: creating a collaborative, memorable customer experience.
Teach your staff to provide “intentional” customer experiences, as these have greater emotional impact and are far more memorable than the delivery of ordinary clinical procedures. My book Quality in Audiology : Design and Implementation of the Patient Experience provides a roadmap for orchestrating these concepts in your practice.
(2) Use motivational interviewing techniques
I am convinced that this form of counseling cannot be replicated by computerized audiometers. It takes a skilled, caring professional to gently nudge many patients toward changing their behavior. The main role of an audiologist is not to dispense a device; it is to facilitate a change in patient behavior. In a clinical paradigm focused on motivational interviewing, the device becomes secondary. If there is one book to read on implementing motivational interviewing techniques in your practice it is Instant Influence by Michael Pantalon.
(3) Employ co-morbidity marketing tactics
Many changes are taking place in the U.S. healthcare delivery model. Audiologists and hearing instruments specialists are well positioned to be valued members of a physician’s team of preventive care experts. This team would consist of representatives of several independent professions, such as chiropractic medicine, optometry, dietetics, and audiology, that provide outsourced preventive health services as determined by patients and their family physician. You can facilitate this change and enhance the productivity of your practice by educating family practitioners and other primary-care physicians about the compelling evidence pointing to relationships between hearing loss and a host of serious medical conditions, including Type II diabetes, cardiovascular disease, and dementia. Every practice should have an on-going “talk-track” with 20 to 50 physician practices in their area, using electronic newsletters and social media. Reading a recent article in ENT Today is a great starting point in developing evidence-based, co-morbidity talking points to share with physicians.
(4) Use social media to create a dialogue with patients
There is a lot of chatter about electronic and social media. I think the real potential of Facebook and Twitter is the ability to bring your database to life. Why not create an on-going dialogue with patients and prospects? It’s a simple as using an app like Zite to create a list of favorite articles and blogs that can be instantly shared with your database on a daily basis.
(5) Customize a value-based pricing strategy in your practice Economists like to say that price is your signal to the market. If you were to try and decode the signal our profession sends to the market, you would find that it that is centered almost completely on a device—one that is quickly becoming just another non-descript commodity. Adopting a value-based pricing strategy will lead you to offer “itemized rehab bundles” of service. By making hearing aids simply one component in the array of services and products available from your practice you signal to consumers that you offer far more than a device they could buy for less at Costco or online. Additionally, using a comprehensive value-based pricing strategy requires practitioners to negotiate more favorable wholesale prices with their preferred manufacturing partners.
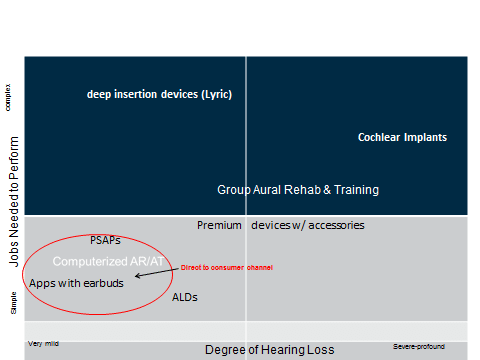
Figure 1. Segmentation matrix with some of the offerings consumers can obtain from hearing healthcare professionals. Readers are encouraged to add more offerings to this matrix.
ATTRACT NEW MARKET SEGMENTS
In addition to providing greater value to the segment of the market you are already serving, it is important to reach new types of consumers.
Conducting small-scale experiments in your practice is a good way to do this. Using the matrix shown in Figure 1 can help you uncover a new segment of the market: Simply divide the hearing-impaired population into quadrants based on the degree of hearing loss and by asking the question, “What jobs do individuals with hearing loss want me to perform?” Notice that the x-axis in Figure 1 is degree of hearing loss. We know that severe to profound hearing losses require different remediation strategies than do milder hearing losses. Now, look carefully at the y-axis. This depicts “the job individuals with hearing loss want us to perform.”
As you can see in Figure 1, the y-axis goes from simple to complex. When you cross these two axes you get a useful four-quadrant matrix that can help you devise a strategy for pursuing an untapped part of the market. Based on some reported prevalence data, we know the number of people with mild hearing loss is quite high. We also know that those with milder hearing loss probably don’t need to be fitted with traditional devices because: (1) their loss is too mild to get much benefit from hearing aids (2) they are asking us to perform a job that traditional hearing aids don’t do very well. Given these considerations, here are two more strategies to use:
(6) Recommend over-the-counter technology
In the lower left quadrant of Figure 1, you’ll see a variety of over-the-counter hearing assistive technology. Such devices can help people who don’t yet use hearing aids deal with hearing loss. Your recommendations need not be limited to PSAPs. You may want to suggest hearing aid apps and computerized brain retraining programs that people with hearing loss pay to download and use. You could even brand these apps with your name and clinic logo.
The goal is to tap into a segment of the market that doesn’t currently take advantage of our offerings and, in time, migrate some of them into the more traditional channel. This model may provide a gateway for some patients to obtain more comprehensive services from you at a later date.
Using the optical industry as an example, we know from a presentation at AudiologyNOW! 2013 (Amlani, Levy, Robbins & Taylor, “Improving Hearing Aid Adoption Rate through Smartphone Applications”) that 20% of patients who bought over-the-counter reading glasses migrated to another customizable offerings like Lasix, prescription glasses, or contact lenses within 15 months.
(7) Tap into the needs of the Healthy Aging Movement
“Baby Boomer” is the popular and somewhat overused phrase used to describe individuals born between 1946 and 1964. A far more descriptive term that defines the behavior of many of these individuals is “Healthy Agers” (also sometimes called “Agile Agers”). Healthy agers can best be described as individuals who want to live to be 100 in the mind and body of a 45-year-old. Many in this demographic group will spare no expense for personalized care and attention in their quest to maintain a high quality of life into their second century.
There is plenty of data showing that healthy agers approach the market in a far different way from previous generations. Reaching these people will require audiologists to band together with other professions to promote wellness among the healthy aging community. Christopher Spankovich’s work at the University of Florida indicates that audiologists are well equipped to advise healthy agers on diet and nutrition. Research like his could even lead to a whole new sub-specialty of Interventional Audiology, which focuses on preventive care of the auditory system.
At the very least, audiologists could become part of a team of healthy aging advisors for individuals wanting to stave off the effects of growing old. Web sites like Vitality Directory might enable you to generate interest from people who want to live to be 100 in the mind and body of a 45-year-old.
Of course, when these healthy agers do take seats in your waiting room, many of the other previously mentioned tactics must be in place if you want to serve their needs.
FINAL THOUGHTS
Hope is not a strategy. It’s time that we stop just waiting and wishing for some new amplification technology to come along that will create a ground swell of new business opportunities. By implementing some of the tactics I’ve recommended that place the professional–not the device–at the center of our profession, we will be one step closer to overcoming the negative effects of disruptive innovations.
Given the sheer number of healthy agers who are beginning to experience hearing loss, we may even see the number of patients waiting to see us skyrocket. To learn more about how to implement these seven tactics in your practice, contact me at brian.taylor@unitron.com. Let the hard work of filling those half-empty waiting rooms begin.
Brian Taylor, AuD, is Director of Practice Development and Clinical Affairs for Unitron. He is also Editor of Audiology Practices, the publication of the Academy of Doctors of Audiology, and the author of the book Consultative Selling Skills for Audiologists, published by Plural.







Great article Brian. I like that you include looping as one way to do outreach in a community. I have been talking about this for nearly 4 years now and several other audiologists even longer than that. Glad to read that looping is going mainstream – read this article here: https://www.audiologyonline.com/ask-the-experts/do-you-explain-recent-increase-11895
I also have wondered why a two dimensional classification system has not been developed; one that designates the severity of the hearing loss (i.e. mild=HL1, moderate=HL2, severe=HL3 and profound=HL4) and one that classifies the degree of word processing difficulties in noise (i.e. QSIN 0-4=1, QSIN 5-8=2, QSIN 9-12=3 and QSIN over 13=4) was never developed. Treatment for a person in the HL2,QSIN1 category is very different, and may even involve over the counter PSAPS, as opposed to a person with a hearing loss in the HL2QSIN3 range. Everyone would then also understand that a person complaining about the benefits of hearing aids with an HL3QSIN4 needs assistive technology, FM systems, auditory training, use of a hearing loop in the TV room and house of worship, while a person complaining even-though he or she scored in the HL1QSIN1 range may not have been fit properly as person in that range would be expected to VERY WELL with amplification. A third dimension could even be added taking the ANL test scores into account. A comprehensive treatment approach could then be developed for each category with clear explanation of expected outcomes. Perhaps a great 4th year AuD student project?
I think creation of barriers to entry will be the nail in the coffin for audiology. Porter who advocated this strategy was wrong and his consulting firm went bankrupt.
The key to filling our offices is creation of a huge base of very satisfied consumers who will become Apostles for hearing aids and audiology. I venture to say with 1,000,000 hearing aids in the drawer we have more terrorists than apostles. Anything short of very satisfied consumers will cause huge brand disloyalty and consumer defection to alternate technology. See https://download.microsoft.com/download/a/e/0/ae0b3074-466e-4876-84d8-dcdf3f928da4/Why_Satisfied_Customer_Defect.pdf
Let’s face it the utility of hearing aids is poor and always has been especially in noise and Far field. And we only have a satisfaction level of about 50% on the phone or watching TV. Why would anyone spend $8000 to just hear in quiet? Few audiologists are willing to provide AR and how many are skilled in tinnitus mitigation? Brand loyalty has never exceeded 50% in this industry. This has little to do with stigma, much to do with accessibility to hearing healthcare for everyone, and a lot to do with our failure to give the consumer substantial benefit at a good value. In addition we have also shown on average no difference in quality of hearing healthcare based on profession (audiologist or dispenser).
We are at a tipping point….that point which you predicted at AAA about 4 years ago.