“Signal & Noise” is a bimonthly column by Brian Taylor, AuD.
It has been estimated that 26.7 million American adults aged 50 years or older have a clinically significant hearing loss with fewer than 15% using hearing aids{{1}}[[1]]. Chien, W. & Lin, F. (2012). Prevalence of hearing aid use among older adults in the United States. Archives of Internal Medicine. 172, 292-203.[[1]]..
By now, most of us are familiar with the PCAST non-binding recommendations, which may eventually culminate in the re-regulation of our industry in order to address this huge unmet need.
It’s this single stat: just one in seven individuals with age-related hearing loss correct the problem with hearing aids.
That is enough to spur any conscientious public health official into action, especially when so much emerging research indicates that untreated hearing loss in adults leaves people at-risk for developing one or more of the sequelae associated with it.
A System Built to Correct a Problem
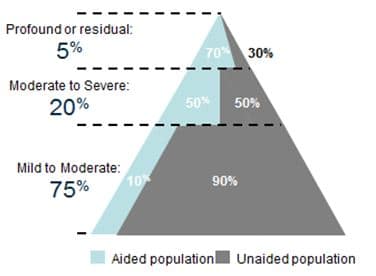
Figure 1. Hearing aid use as a function of degree of hearing loss.{{4}}[[4]]Wallhagen, MI & Pettengill, E. (2008). Hearing impairment: Significant but underassessed in primary care settings. J Gerontol Nurs. 34: 36-42.[[4]] ,{{5}}[[5]]Lin, F. et al (2011). Hearing loss prevalence in the United States. Arch Intern Med. 171.[[5]],{{6}}[[6]]Nash, SD et al (2013). Unmet hearing health care needs: The Beaver Dam Offspring study. American Journal of Public Health. 103, 6, 1134-1139.[[6]]
It’s not surprising that the greater the degree of hearing loss, the more likely it is that a patient will possess hearing aids. These patients, after all, are likely to have a handicapping condition warranting traditional amplification and its accompanying professional services. Their hearing losses are more complex and they typically require more time and expertise to address.
The current clinical system – the workflow, the tests we conduct, predicated on multiple office visits over time – has been built to address the needs of the top 25% of the triangle in Figure 1. It’s a relationship-based transaction.
Yes, this relationship-based transaction needs improvement, and, like all matters related to healthcare, it could benefit from greater efficiency and more effective communication. But, on average, we do a decent job of delivering these products and services to the patients who value it.{{2}}[[2]]The delivery of patient centered care undoubtedly could be improved. See Grenness, C., Hickson, L., Laplante-Lévesque, A., Meyer, C., & Davidson, B. (2015). The nature of communication throughout diagnosis and management planning in initial audiologic rehabilitation consultations. Journal of the American Academy of Audiology, 26(1), 36-50 to learn how many audiologists gravitate toward discussion of technology and do not practice patient centered care.[[2]]
A System in Search of a Problem to Solve
Products and services that work relatively well for the top 25% of the triangle, however, do not effectively address the wants and needs of the other 75% of adults with hearing loss. It’s no wonder that only 10% of them possess hearing aids: the process of obtaining them, and their price, are not in alignment with the needs of this group.
For the vast majority of these individuals, they don’t have a “problem” to be solved, but some type of daily function that needs to be enhanced or improved. It could be a certain meeting where the boss’s voice is unclear or perhaps it’s talking on their mobile phone; it might even be that PBS television program with British accents that causes a lot of frustration.
Whatever the difficulties and challenges they are normal for the individual’s age – they just don’t hear like they did 10 years ago. Some recent data we collected and analyzed on more than 100 Australian adults of working age indicates that approximately 60% of them had self-reported mild to moderate levels of difficulty in specific listening situations and completely normal audiograms.{{3}}[[3]] Taylor, B., Manchaiah, V. & Clutterbuck, S. (unpublished data) Patient Assessment of Communication Abilities (PACA): Communication difficulties experienced by working adults with normal audiograms.[[3]]
A New, Alternative System for the Many
Next week’s post will pickup where this post leaves off, looking to changes in regulation and delivery systems to meet the needs of the 75%. Those changes offer new opportunities for audiologists to develop and participate in a new arms-length value proposition to stimulate demand for improving hearing difficulty.
Brian Taylor, AuD, is Senior Director, Clinical Affairs, for Turtle Beach/Hypersound. He continues to serve as Editor of Audiology Practices, the quarterly publication of the Academy of Doctors of Audiology. During the first fifteen years of his career, he practiced clinical audiology in both medical and retail settings. Since 2005, Dr. Taylor has held a variety of leadership & management positions within the hearing aid industry in both the United States and Europe. He has published over 50 articles and book chapters on topics related to hearing aids, diagnostic audiology and business management. Brian has authored three text books: Fitting and Dispensing Hearing Aids (co-authored with Gus Mueller), Consultative Selling Skills for Audiologists, and Quality in Audiology: Design & Implementation of the Patient Experience. His latest book, Marketing in an Audiology Practice, was published in March, 2015. Brian lives in Golden Valley, MN with his wife and three sons. He can be reached at [email protected] or [email protected].
feature image courtesy of Cambridge in Color