“Signal & Noise” is a bimonthly column by Brian Taylor, AuD.
In addition to fitting conventional hearing aids, audiologists and hearing instrument specialists may have the opportunity to adapt an à la carte approach to technology with a menu of offerings tailored to the “just good enough” needs of the individual. This menu may include PSAPs, hearables, devices like Hypersound, and even the stand-alone delivery of therapeutic services, which could be centered around cognitive behavioral counseling and motivational interviewing.
In short, the ability to provide truly patient-centric care that revolves around the behaviors and attitudes of the individual, rather than a single device. Lower prices for medical devices need not mean less advanced technology or inferior service. They could reflect using more simple-to-use gadgets, specialized for specific purposes – a device for the phone, one for TV and home audio, and ear-worn devices for conversations outside the home. All simple-to-use, high-quality and customized to the patient by their audiologist, who serves as the hub.
A New Delivery Model, A Larger Market
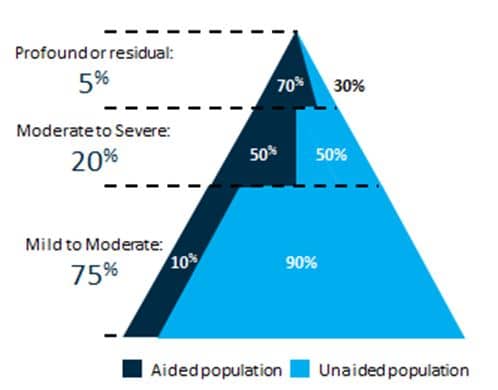
Fig 1. Hearing loss segmented by degree. Data from Nash (2013)1, Lin et al (2011)2, Lin (2011)3, Wallhagen & Pettengill (2008)4
With a new delivery model, we may reach the vast majority of individuals with milder losses, who rarely consult us for services. Historically, our industry has served the top 25% of patients in Figure 1. These are individuals, older in age, often with more complex problems, requiring more time and expertise to manage.
On the other hand, those in the bottom 75% of the pyramid are likely to have less complicated hearing loss that doesn’t require numerous appointments for adjustments and counseling. “Just good enough” will probably appeal to this large group of patients. But our current system, predicated on numerous office visits and incremental improvements in hearing aid features isn’t valued by the vast majority of patients in the bottom three-quarters of Figure 1.
It’s Hard, But We Have to Change
The demand for “just good enough” will require us to change. And, we all know change is never easy. After all, the majority of hearing care professionals still do not routinely use speech-in-noise tests or validate outcomes – even in the face of overwhelming evidence supporting their use.
If Roger’s Diffusion of Innovation Curve holds true, it will take 50% of us to embrace a new approach to patient care before it becomes standard practice. The shifting needs of the market, however, are apt to force us to change. If audiologists and hearing instrument specialists want to thrive in the “just good enough” era the majority of them will have to change.
Collectively, we need to engage in “change talk,” which, ironically, comes directly from the process that clinicians who practice motivational interviewing use to elicit behavior change in their own patients. There are three important aspects of change talk and each of them will help us navigate the uncertainty of the present era:
- Do we recognize the need to change and how important is it for hearing care professionals to evolve in order to meet the changing needs of the marketplace?
- Confidence: Do we have the necessary skills to meet the demands of consumers, and how confident are we in mastering these new skills?
- Commitment: How committed are we to changing? Who is going to lead this unified commitment to change?
Even though technology is fast becoming a commodity, the uniquely human skills of providing guidance and support based on sound scientific principles and good audiology cannot be commoditized by machines – yet. It all starts with our desire to change in order to meet the needs of the marketplace in the “just good enough” era.
This is the second post in the “Signal & Noise” series. Click here for Post 1 or Post 3.
References
1Nash, SD et al (2013). Unmet hearing health care needs: The Beaver Dam Offspring study. American Journal of Public Health. 103, 6, 1134-1139.
2Lin, F. et al (2011). Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol A Biol Sci Med Sci. 66: 582-590.
3Lin, F. et al (2011). Hearing loss prevalence in the United States. Arch Intern Med. 171
4Wallhagen, MI & Pettengill, E. (2008). Hearing impairment: Significant but underassessed in primary care settings. J Gerontol Nurs. 34: 36-42.
Brian Taylor, AuD, completes his work this week as Director of Practice Development & Clinical Affairs for Unitron. He continues to serve as Editor of Audiology Practices, the quarterly publication of the Academy of Doctors of Audiology. During the first fifteen years of his career, he practiced clinical audiology in both medical and retail settings. Since 2005, Dr. Taylor has held a variety of leadership & management positions within the industry in both the United States and Europe. He has published over 50 articles and book chapters on topics related to hearing aids, diagnostic audiology and business management. Brian has authored three text books: Fitting and Dispensing Hearing Aids (co-authored with Gus Mueller), Consultative Selling Skills for Audiologists, and Quality in Audiology: Design & Implementation of the Patient Experience. His latest book, Marketing in an Audiology Practice, will be published in March, 2015. Brian lives in Golden Valley, MN with his wife and three sons. He can be reached at brian.taylor.aud@gmail.com.
feature image courtesy of biederman blog







