by Amyn M Amlani, PhD
A few weeks back, I spent the afternoon shopping for clothes with my 14-year-old daughter. As we made the rounds at the local mall, I was surprised at how elaborate a consumer my daughter had become. Outfits that I assumed were a “slam-dunk” purchase were rejected, and other outfits that I thought were a “no-way” purchase were deemed acceptable. I also noted that purchase intent was further influenced, both positively and negatively, by the interactions she encountered with the salesperson.
On the ride home, I inquired about my daughter’s shopping philosophy. During our discussion, it was apparent that her purchasing behavior was tied to risk preferences, with risks stemming primarily from peer acceptance, self-appearance, social status, perceived value, and brand name.
My teenage daughter’s purchase decisions are not much different from the average adult listener seeking treatment options from their local hearing healthcare provider. That is, impaired listeners uptake of audiology services and technology increase when risk preferences are low for similar traits (i.e., peer acceptance, self-appearance, social status, perceived value).
This month’s blog delves into purchase intent through the lens of a managerial economics concept called risk preference and its potential application in the clinic.
Risk Preference – What is it?
Risk preference refers to the attitude people hold towards risks. The perception of risk, which varies among individuals, influences whether a product or service is purchased.1-2
The goal of the supplier (e.g., hearing healthcare provider) is to assess each individual’s risk preference towards an outcome. Having knowledge of this data affords the supplier with a means in which to temper risks perceived by the end user.
For example, the provider’s knowledge of a patient’s heightened risk towards being amplification and social acceptance could lend to the additional counseling, a recommendation that the patient and family member attend an in-house group audiological rehabilitation, or both.
Risk Preference – How is it Determined?
Risk preference is determined by quantifying an individual’s subjective utility function, measured in utils, for each given outcome (e.g., self-appearance, social acceptance, stigma, empathy, trust, shared decision-making). The utility function of each outcome is then summed together yielding a composite score.
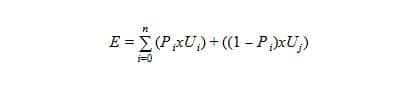
The utility function is comprised of two alternative outcomes (also called payoffs), A or B. Outcome A occurs at one probability (P) and outcome B occurs at a second probability of 1 – P. The equation for determining risk preference outcomes is:
where E represents the utility factor, Pi signifies a given probability Ui denotes the utility value of outcome A, and Uj denotes the utility value of outcome B.
Clinical Application
Let us assume that we assess a utility function for patient risk preference before and after an initial audiologic consultation. Prior to the consultation, the patient is asked to complete a short 15-item survey where he/she places a value—between 0 and 10—for each expected outcome (e.g., self-appearance, social acceptance, stigma, empathy, trust, shared decision-making).
The composite score of the pre-consultation survey responses is then entered into the equation as outcome A, and the value of 0—a reference point—is used as the value for outcome B. As an example, assume outcome A yields a composite score of 90, outcome B is 0 (i.e., reference), and the probability of adopting audiological services and technology is 50%. These data yield a utility factor of 45 utils (i.e., (90 x 0.5) + ((1-0.5) x 0)).
At the conclusion of the initial consultation, the patient is asked to complete the same survey that was provided at the pre-consultation. Assume that the sum of the post-consultation survey equals 125. In the equation, outcome A is 125 (from the post-consultation survey), outcome B is 90 (from the pre-consultation survey), and probability of adopting audiological services and technology remains at 50%. The utility factor results in a value of 107.5 utils (i.e., (125 x 0.5) + ((1-0.5) x 90)).
Risk Attitudes and Buying Behavior
Attitudes toward risk varies among individuals, and is prone to shifting between pre- and post-exposure based on interactions with the supplier’s environment and personnel. The changes in attitude are grouped into three categories:
- Risk taker – Describes that individual who is most likely to move forward with uptake of services and technology. This individual is identified because their post-utility factor is markedly higher than their pre-utility factor (i.e., the example provided above, where pre- and post-utility factors were 90 and 120, respectively).
- Risk neutral – Describes that individual whose pre- and post-utility factors are essentially unchanged (e.g., pre- and post-utility factors of 90 and 100, respectively). In this case, the individual is indifferent about uptake. An assessment of their survey responses might identify an area(s) of doubt, and identifying this/these area(s) provide(s) an opportunity for counseling, audiological rehabilitation, or both. The pre- and post-data analysis could also lend insight regarding the provider’s demeanor with their patients.
- Risk adverse – Describes that individual whose post-utility factor is less than the pre-utility factor (e.g., pre- and post-utility factors of 90 and 60, respectively). In this case, the individual will not be adopting audiological services and technology. Like the risk neutral category, the provider should review the pre- and post-survey responses to identify counseling opportunities and self-reflection of provider demeanor.
Summary
The concept of risk preference can be implemented as a clinical tool that provides insight into purchase intent and the patient-provider experience.
Based on the patient’s response, the provider is now better equipped to manage patient attitudes towards treatment uptake using additional counseling and audiological rehabilitation. In addition, patient responses allow for the provider to self-reflect on their demeanor.
References
- Weber, E. U., & Milliman, R. A. (1997). Perceived risk attitudes: Relating risk perception to risky choice. Management Science, 43 (2), 123-144.
- Weber, E. U., Blais, A. R., & Betz, N. E. (2002). A domain-specific risk-attitude scale: Measuring risk perceptions and risk behaviors. Journal of Behavioral Decision Making, 15 (4), 263-290.
*featured image courtesy USAF








Enjoyed this post but am wondering how you feel about the COAT. I’ve used it successfully in the past but have gotten away from it. With increased demands on our time clinically do you think the COAT and your approach will yield similar results? I ask simply to avoid having to learn a a new tool to accomplish the same goal. Patient motivation is key to success in my opinion and the COAT was usually a pretty good indicator of their motivation.