I never grew up wanting to be an audiologist. It just sort of happened.
Like so many people in my profession, I stumbled across audiology by complete accident. After changing my mind probably about a dozen times during my first two years of college, I finally decided on a major: Psychology. I always found the brain fascinating and learning why people do the things they do just sounded like fun.
I distinctly remember sitting in my first class as a newly-minted Psychology major. I was sitting near the back of a lecture hall with about 500 other students at Washington State University (WSU), squinting to see the professor standing in the front of the room. I began to look around and thought to myself, “what exactly will I be able to do with a degree in psychology?” I started to panic: Had I made the right choice?!
I began to wonder… “maybe I should start looking into a different career, so I don’t have to spend my entire life going to school.”
Through some investigation I realized that a Ph.D. was likely going to be necessary for a “real” career in psychology, or so I thought at the time. Little did I know then, I would ultimately be committing 8 years to my post-secondary education.
The Love-Hate Relationship Begins
I discovered audiology after browsing the course catalog offerings at WSU and never looked back. I completed my AuD degree at Western Michigan University and have happily worked in a private practice setting ever since.
I LOVE being an audiologist.
I LOVE helping patients… There are few things as rewarding as improving a person’s quality of life through better hearing. At this point, I honestly couldn’t imagine doing anything else.
However, one thing I do HATE about my chosen profession is the debt. While I don’t want to sound ungrateful for being employed and having a great career, paying back the sizable loan debt I accrued as a student means less discretionary income at the end of each month for the foreseeable future. Even with my part-time gig as a research assistant for 3 years, I still had to borrow from Uncle Sam to finance my education.
In the clinic, most of my patients know me on a first-name basis, so I could honestly care less about the formality of being addressed as “Doctor.” However, one of the issues many of us neglect to discover until after graduation is how audiologists are often viewed as DINO’s or “Doctors-In-Name-Only.” Despite years of clinical training and expertise in the auditory and vestibular system–lack of full autonomy, low earnings, and frequent classification and treatment in the medical community as “ancillary” professionals would sadly indicate we remain DINO’s in many respects.
With such abysmal reimbursement for our services, it’s no wonder our profession’s median earnings are on more on par with Dental Hygiene rather than that of Dentistry (which happens to be one of the professional doctoring models audiology was attempting to emulate with the advent of the AuD degree). While we can debate the root cause of this, that’s just the reality.
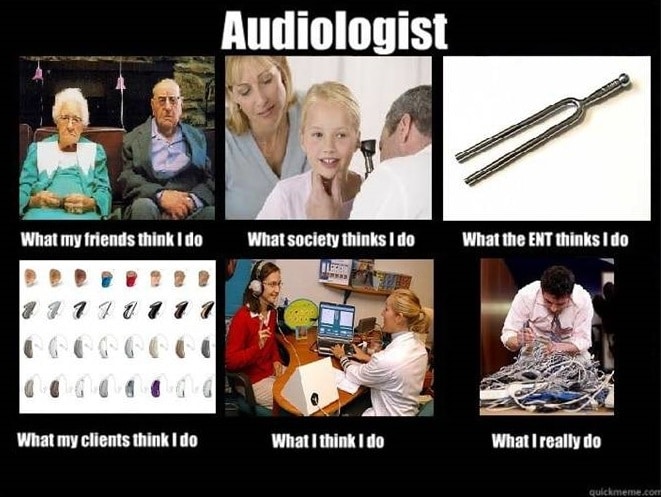
Found Humor{{1}}[[1]]”Found Humor” courtesy of r/audiology at imgur.com[[1]]: Can you relate to this?
Life in Audiology
Let’s face it, in audiology the internal rewards are tremendous: Have you ever seen a child dance in the office and laugh hysterically after hearing his own footsteps for the first time? It’s pretty awesome.
For all those grumpy patients we might see in a week, we keep going back to the clinic everyday for those patients who tell us how happy they are after following our advice on getting hearing aids (or a cochlear implant) or maybe after we helped them resolve a chronic vertigo problem they’ve suffered with for many years. That’s definitely the most gratifying part of being an audiologist for me.
It’s those external rewards, however (i.e., reimbursement/compensation), that remain stubbornly low for many in the profession.
I had a clinical preceptor once tell me, a direct quote from her ENT physician employer,
“Why do audiologists need a doctoral degree? Are you guys trying to educate yourselves out of a job?”
As expected, my preceptor was pretty offended by her employer’s comments. Although, maybe this was a fair question.
Should we be afraid to ask ourselves if we are on the right path as a profession? Are we simply over-educating ourselves and financially burdening the next generation of audiologists? …or, as some would claim, are we instead laying the groundwork to prepare for a future of greater autonomous practice and ownership of the profession?
The jury is still out.
As I take the reins as the new editor of Hearing Views I promise to tackle these issues and many others that are relevant to audiology, the hearing industry and the broader Hard-of-Hearing community. I look forward to sharing with you.
Up next: the dish on debt. We revisit our series on the high cost of audiology education.
Featured image photo courtesy of Stuart Miles at FreeDigitalPhotos.net.








If one looks closely, there are medical lab tests that reimburse at the $4 to $5 level. They came into being in the 1950s and 1960s. Our 92557 also was “born” about that time. To suggest that reimbursement for this test code alone is insufficient is a little like a physician complaining that typing a blood sample doesn’t pay enough to keep him/her in practice. What’s the lesson here?
Mike, I think I get what you’re saying, and I was simply providing the example of the hearing evaluation to illustrate my point that audiology services are not well reimbursed in general–now we can get into a whole other conversation about fee for service and many of these related issues, but that’s best left for another day.
However, your analogy isn’t a truly fair comparison to the situation in audiology (lab test vs. hearing evaluation). Unlike a medical physician, I cannot “order” a hearing exam without conducting it myself. A physician has a technician or nurse take blood, send it to lab, etc, and then the physician gets the results and discusses with the patient. For better or worse, this just isn’t how it’s done in our profession. A billable diagnostic hearing evaluation requires an audiologist to perform the procedure: as you know we cannot bill ‘incident to’ and have a technician perform the service.
The ENT physician employer who said, “Why do audiologists need a doctoral degree? Are you guys trying to educate yourselves out of a job?” must view audiologists as “their” ancillary personel and wants to keep us under their control. One of my dear ENT friends once told me, “Larry, I went into my profession and was trained to do the work of an ENT physician. As such, I should be able to have a great career and make a good living doing so. You went into audiology and was trained to do the work of an audiologist. As such, you should also be able to have a great career and make a good living doing so.”
If the audiology programs/professors are training and professionally socializing students properly, young audiologists should be prepared to enter their role in the healthcare arena as general practitioners who are the point-of-entry doctors for hearing and balance care (ENTs are tertiary providers). The profession’s efforts, politically, legally, financially, etc. should be commensurate with this goal for our profession. To not work diligently to position audiology and audiologists into this slot is to consequently position us to remain floundering in the healthcare hierarchy subjecting the profession to the manipulation by other non-audiologists. If the profession gets this right, you will see a positive effect on income.
Larry
Well said Larry, thanks for your comments!
Great post. I would argue that the AuD Movement was not completed with the formation of the AuD degree. Recognition of our profession (both under Medicare as well as in the overall healthcare community) has not budged. As you aptly point out, every new audiology graduate is faced with that fact from a financial and professional perspective. I encourage anyone who is motivated to take these issues head on to review the 18×18 Movement at 18×18.org. These battles are never quick or easy, but as we all know to well, they are absolutely essential. Thank you Kevin for discussing this incredibly important topic.
Thank you Brian. Yes, amazingly our status under Medicare hasn’t budged, despite being in the 3rd decade of the ‘AuD movement’. However, we have made slow and steady progress on many fronts over the years in the profession and hopefully we will see a time in the near future where this status has changed.
Direct Access/LLP status for audiologists was essentially one of the main objectives/intents behind the the creation of the AuD degree in the first place (not a ‘radical’ new idea as some have suggested). Audiologists and AuD students would be well served to review issues such as 18×18 and find out where our different organizations stand on the topic of autonomy/scope of practice so they can judge for themselves which strategy they should support (unfortunately, all of our organizations are supporting separate strategies).