By Brian Taylor, AuD, Editor-at-Large

Brian Taylor, AuD
In the dystopian HBO series Westworld, android “hosts” cater to high paying “guests” (humans) of a Wild Wild-themed amusement park. The hosts are so proficient at copying human emotions, they have the ability to replace humans.
Given all the advances in AI-driven hearing screening and hearing aid adjustment capabilities that seem to be ramping up as a result of Covid 19 physical distancing measures, it would be easy to assume that hearing-related services, like Westworld is being on the path to replacement by robots. As we will see, be not afraid fellow humans, we are indispensable.
To appreciate just how indispensable humans are in the process of quality hearing services, let’s go back a few short years. In a 2017 Cochrane Review article, Melanie Ferguson and colleagues conducted a systematic meta-analysis on the effects of hearing aid use on communication in everyday life for adults with mild to moderate hearing loss. The authors uncovered five studies involving 825 adults, all randomly provided either hearing aids, no hearing aids or placebo hearing aids.
Unsurprising to most clinicians, they found evidence in three studies that hearing aids have a large beneficial effect in improving the ability of adults with mild to moderate hearing loss to take part in everyday situations. Additionally, they found hearing aids “provide a small benefit to improving general health-related quality of life, such as physical, social, emotional and mental well-being, and have a large effect in improving the ability to listen to other people.”
Their thorough analysis of the data, and conclusions they draw from it, run parallel with several other studies published since then (see this 2018 JAGS study as one example) that indicate expertly fitted hearing aids not only help people communicate more effectively, they also have several benefits that impact health-related outcomes, such has slowing the trajectory of cognitive decline, lowering the risk of falling and lessening the ill-effects of social isolation. Even more recently, University of Toronto researchers attempted to describe the complex association between hearing loss, hearing aids use and quality of life measures.
Using a bottom-up approach that relied on feedback obtained directly from persons with hearing loss as well as clinical experts, Dixon and colleagues revealed a long list of common themes associated with quality of life and hearing aid use, including communication, social relationships, emotion, work function, independence, listening to music, talking on the phone, and listening effort. The analysis also uncovered several negative effects associated with quality of life resulting from hearing loss, such as tinnitus as well as stigma and discomfort associated with having to rely on instrumentation placed on the ears to improve communication.
Their work, published on May 14 in JAMA-Otolaryngology lays the groundwork for hearing-related quality of life measures that can be used clinically, we hope, in the near future.
Benefits of Treating Hearing Loss
It is good news, of course, that wearing hearing aids is evidentiarily linked to both improved day-to-day communication and several health-related outcomes that contribute to a better overall quality of life. However, this link between hearing aid use and beneficial outcomes is predicated on two important factors:
- Persons with hearing loss must take an active role is seeking treatment, and
- Persons with hearing loss must wear their hearing aids consistently every day to experience these benefits.
Over the last few years, and certainly hastened by the Covid-19 pandemic, a wide range of AI-based tools that screen hearing and automate certain aspects of the fitting and fine-tuning process are readily available on smartphone apps. Many of these tools are based on solid clinical evidence and actually work quite well.
Some recently published studies, however, hint that AI-driven, technological solutions geared toward addressing the two factors listed above have some limitations and might work best when placed into the hands of an actual human being – one with empathy and expertise in hearing loss and hearing treatments who decides along with the patient when to lean on these automated, tech-driven tools. First, let’s look at how technology could enable more persons with hearing loss to actively participate in the treatment process.
In a recent study, published-ahead-of-print in the American Journal of Audiology, Danielle Schonborn and colleagues investigated the help-seeking behaviors of individuals who failed an app-based hearing screening test. One of the key results of their study was that 86% of those individuals who failed the hearing screening, and requesting to be contacted by an audiologist for follow-up, did not initiate any further action with the clinic. Additionally, of the 3,000 or so who failed the self-guided hearing screening and did not follow-up with the clinic, 51% of them did not believe they had a hearing loss.
The results of this study suggest that clinicians cannot simply rely on self-guided gadgetry, no matter how cool, to bring more help seekers into the clinic. Basic blocking and tackling, like educating the community about hearing loss prevention and importance of periodic hearing checks, guided by an empathic human being with an expertise in hearing loss and hearing treatments is an essential part of the equation.
Now, let’s examine the second consideration: enabling persons with hearing loss to wear their hearing aids more consistently so they can experience all the beneficial outcomes associated with their use. A recent article, using survey data collected in Wales, UK and published in June by the International Journal of Audiology reported that 20% of adults do not use their hearing aids at all and 30% use them just some of the time.
As the lead author, Harvey Dillon, stated in an accompanying press release, “Although under-use or non-use of treatments by some patients is by no means unique to hearing aids, achieving uniformly high use of hearing aids by those who need them would provide a major benefit to society. We already know that the largest predictor of hearing aid benefit is the quality of interaction with the health professional, rather than the degree of hearing loss. But it’s imperative that more research is done to understand why non-use can set in so quickly for some and devise efficient procedures to prevent this from happening.”
Two additional studies also suggest there is plenty of room for improvement when it comes to increasing the overall wear-time of hearing aids. Rebecca Bennett and colleagues investigated the prevalence of device-related problems associated with hearing aid use. In their survey of more than 400 adult hearing aid owners, they found 98% of respondents reported over the course of 1-2 years at least one problem with their hearing aids and more than half of this group (54%) did not report the problems to the clinic. The three most widely reported problems were difficulty hearing in noisy environments, hearing in windy environments, and understanding certain voices.
Perhaps the most eye-opening finding was the mean number of problems reported by each hearing aid owner was 10. A finding that suggests solving problems more quickly when they first occur as well as more effective use of time helping patients many months after an initial fitting are important. Tasks more readily accomplished when face-to-face appointments are blended with remote teleaudiology options.
Traversing the Digital Divide
Lastly, the series of MarkeTrak 10 papers, published earlier this year in Seminars in Hearing continue to be a treasure trove of information for conscientious clinicians. One of the more remarkable findings published in the MT10 paper authored by Erin Picou was that a growing number of patients have wireless capabilities in their hearing aids (54% in MT 10 compared to 43% in MT 9) while 20% didn’t know if they had wireless technology in their hearing aids.
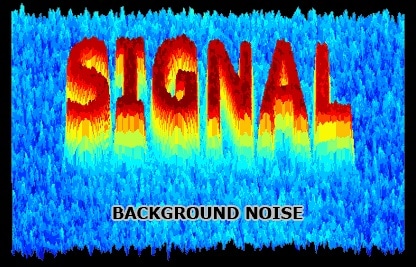
However, this wireless technology–proven to be effective in background noise and other challenging listening situations–continues to be under-utilized.
Picou reports that 68% of owners do not have a downloadable smartphone app compatible with their hearing aids, 79% don’t have a TV streamer, and 80% don’t have a companion microphone. Yet, of the 15 to 20% of owners who actually possess these newer features, about two-thirds report they use them a lot — percentages that tell us we need to spend more time teaching, empowering, coaching and encouraging our patients. Things humans are good at.
The results of these recent studies remind us that no matter how cool or how effective AI-based technology becomes, it is the relationship between the person with hearing loss and the provider that drives much of the outcome.
A recent series of NAL webinars with the catchy title “Soundbites” can be found on YouTube. As some of the NAL Soundbite researchers have so articulately shown, it not about the technology, its about the ability of the clinician to use the technology to facilitate feelings of empowerment and boost self-confidence so that persons with hearing loss actively participate in the process of taking action and becoming all-day every day wearers of hearing aids.
Brian Taylor, AuD, is the director of scientific and product marketing for Sivantos. He is a veteran of the hearing industry with more than 25 years of experience, most recently at Fuel Medical Group where he served as Director of Clinical Audiology. An Audiologist since 1991, Brian received his Au.D. from Central Michigan University in 2006. During his career, Brian has been involved in many areas of the industry including clinical practice, practice and professional development, and training. Brian is a prolific and respected contributor to the industry with more than 25 publications and numerous speaking engagements both domestically and internationally. He has written and edited six textbooks, and most recently authored Essential Business Principles and Tactics for Clinical Managers: The First (or Next) 100 Days. Brian served as Editor-In-Chief at HHTM from 2018-2019 and currently serves as Editor-at-Large.