Editor’s Note: Terry MacTaggart continues his discussion on how we can better serve our customers – persons coping with hearing loss and communication challenges during one of the most uncertain moments in our lifetimes. Click here to view Part 1.
Why are so many people left out?

Terry Mactaggert
There are several well-known reasons – stigma of older age, access to services and acquisition cost of products being the major ones. These are well documented in the literature and summarized in the Academy of Sciences report and the subsequent Congressional Act of 2017 which mandated a new class of over the counter hearing devices.
While wireless wearable devices have become commonplace and miniaturization and performance improvement of hearing instruments continues to occur, promotion by the industry still focuses primarily on older people who become “patients” even though this label plays into an emotional bias held by many against such messaging. Inadvertently perhaps, this leaves behind the tens of millions who are earlier on in their journey yet clearly experiencing hearing change.
Reliance on bricks and mortar clinics as the major distribution source staffed by relatively few professionals compared to the need also weighs in heavily. Participants are often compelled by ownership or financial arrangements with suppliers to perpetuate the existing limited access, high price model.
Family physicians know their patients and are well positioned to perform a key “gatekeeper” role but they often lack the training and tools as well as the connections and confidence to refer to local dispensers.
If the system was operating effectively, establishing a baseline hearing profile for everyone over 40 and under 12 would be as commonplace as tracking blood pressure. In the majority of medical practices we have worked with, 70% or more of the patient roster should have their hearing tested given age and/or lifestyle and/or co-morbidities.
The hearing industry is also one of the last anywhere to bundle upfront in the price of a device a number of future services rather than allowing the buyer to select and add what he or she believes may be needed. Students of industrial structure would argue that this is very unusual – a function of the market power and scarcity of alternatives the industry has traditionally enjoyed.
The net result with few exceptions is the “sticker shock” that consumers typically experience when confronted by pricing.
What is the Experience of Those Using Hearing Instruments?
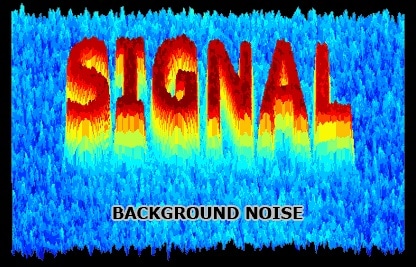
The simple answer is “mixed” at best. About 25% of those who purchase hearing aids don’t use them after a period of trial. Reasons include lack of comfort, frequency and expense of service required, encroachment of background noise and one that is prime – inadequate orientation, training and support.
Aided hearing requires the wearer to persevere while experiencing a new way of processing sound. Many find this hard to adapt to and abandon the effort. Basically the hassle of instrument use outweighs the perceived benefit to be gained.
How and Why is the Hearing Environment/Market Changing?
There are obvious, now evident signs. Deregulation is a leading indicator as are the growing number of companies reaching out to consumers directly with less expensive devices. An encouraging, if hard to completely isolate factor, is what appears to be a growing awareness among the public about the importance of hearing health.
One explanation is simply to note that we are living in the 21st century rather than the 20th where the Internet, Mobile Me and Medicine 3.0 are increasingly apparent.
Consumers are more sophisticated and capable of taking control of their health and well-being with new tools that are increasingly being made available. Systems that are perceived to be closed, offering solutions at high prices, are less favored.
What do Consumers Typically Want from a Product or Service?
This is a central question, one that as a participant/observer of the industry, I’m not confident has ever been adequately addressed.
We certainly have a handle on what most providers (the dispensing audiologist or HIS) respond to but what about the consuming public at large? While some might argue the point, preoccupation by the industry with product development and selling to its distributor channel has limited gaining a comprehensive and dynamic appreciation of what the ultimate customer expects and is motivated by.
Applying Marketing 101 suggests there are seven factors that make a product famous, nurturing trust, loyalty and recommendation. These are summarized as…
- Quality of pitch – Clear information about what the product or service is and how it is used – its utility.
- Reliability – What you see, read or hear about is what you actually get.
- Convenience in use – Competent direction leading to trouble free application.
- Ease of acquisition – Few, if any, hoops to jump through; no surprises or tricks.
- Try before you buy – Ideally a chance to experiment and experience before paying.
- Post acquisition support – Particularly important when installing or adjusting to the product or when service is complex.
- Warranty – Hassle free recourse if the product or service doesn’t work effectively.
Other lessons from the front lines often include…
- Just don’t talk at customers, teach them!
- Listen and learn as much as you teach…
- Acknowledge shortcomings and mistakes…and move quickly to correct them.
A credible argument can be made that leading suppliers and top practitioners rank quite well when these performance criteria are applied. My personal rating on a 10-point scale lies in the 7.5 to even 8 range. At a guess, that would likely decline by at least two points should the industry as a whole ever be measured (Full disclosure – I tend to be a hard marker).
Recall too that we’re referring here primarily to the hearing aid aspect of the industry, rather than the full sweep of hearing health. Our hearing triage indicates that that cohort represents about 30% of those who have tested. In engaging consumers, it’s critical to consider the needs of the entire target group and adopt a broader perspective.
That’s where our new North Star is located!
What do Consumers Need (even if many are not aware of needing to want it)?
This is where the rubber hits the road if you buy into the Basic Premise – i.e. that excluding so many from the hearing health system represents a growing public health issue; and to fix it requires more than a 20th century bricks and mortar solution. That notably is out of tune with the times and will not come close to providing the necessary reach.
Consider what’s becoming commonplace in other fields of healthcare and wellness. Recent science combined with virtual means of detection and treatment are available in a growing number of areas. “E-patientry” and the younger doctors supporting it, began to emerge almost ten years ago. MedTech is now one of the hottest categories in the professions as well as the investment community. Hearing health has lagged rather than lead these innovations.
Applying such lessons widely and making a hearing health process of high quality available to millions of people is undoubtedly daunting but not impossible to achieve. Or at least to work aggressively towards.
We take as a given the importance of understanding and becoming proactive about one’s hearing status as well as the incidence of hearing change in the general population. It’s similar to what we have learned with the COVID dilemma, however. Without adequate testing (and testing 2%-4% of the relevant population is clearly inadequate) we can’t make any significant advance in confronting the problem.
As a first step, therefore, providing easily accessible and reliable testing via the Internet using any device, anywhere, at any time is fundamental.
Then comes the equally important question of trustworthy evaluation, recognizing that such classification will be preliminary but still indicative. It is here that inadequacies are apparent – the traditional 25db threshold for normality across the three frequency speech range of an audiogram does not account for its pattern or the subject’s medical history; its also ignores any measure of confidence that a seasoned audiologist would apply. Taken to its extreme (commonly experienced – just try the great majority of tests available on the Internet), it often leads to the promotion of a hearing instrument – what some refer to as “Click Bait”.
Trolling for low hanging fruit, even with “audiological support” is now de rigeur. The objective almost without exception is to sell yet another device. Critics recognize this as “weaponizing” the test. Using our 10-point scale, this approach would warrant no more than a 3.
When properly tested and evaluated, preliminary hearing triage becomes possible – i.e. the subject’s hearing status can be classified into standard audiological categories. Our data sets indicate that about 80% of the population represent routine cases – they are relatively easy to treat. 20% are complex. A minority – about 30% on average – have or are trending towards what appears to be a permanent sensorineural problem and should consider a hearing device with appropriate guidance. Another 20% appear to be treatable (Conductive indication) and, if constant, should take action at home and in consultation with their family doctor. The remainder indicate either a Normal pattern and level (the largest category who should keep testing themselves periodically) or Mixed (something is going on, possibly a combination of conditions that can’t be separately classified signalling that a full work up is warranted).
In every case it’s appropriate that the family physician be kept informed given his/her experience with the patient, knowledge of the patient’s chart and co-morbidities. Using hearing protection when exposed to loud sound is also paramount.
The key we believe to addressing a very wide audience (not just the obvious segment – older with more advanced sensorineural losses the industry concentrates on) involves providing an attractive and inexpensive hearing health package consisting of five components – testing, classification and triaging, pointing towards best next steps given a person’s hearing status, making coaching about hearing available including connections when needed to medical and audiological talent, and, if appropriate, providing access to products and services that could be helpful. That combination represents a MedTech Solution that avoids bias.
It’s the closest thing to “personalized medicine” one can achieve for hearing. And is a few steps beyond what has generally been available to date.
The flow chart below illustrates this hearing health pathway.
Hearing Health Tech involves a five-step process designed to educate and empower the consumer about taking control of his/her hearing status.

It’s an End-To-End process incorporating effective methodologies, easily understandable guidance and, when requested, reliable advice and solutions.
**Click here for Part 3: Concluding remarks on what this means for the industry and where we go from here.
Terry Mactaggart is the President and CEO of Ultimate Kiosk Inc. and Summus Hearing Solutions Inc., AI-enabled software companies with proprietary technologies aimed at capitalizing on opportunities in international hearing health. He has substantial experience with private venture creation, financing and growth as an investor, consultant, director, chairman and president of a number of companies – both privately owned and publicly traded – as well as of a private equity fund. A broad international perspective has been gained from these activities as well as from his leadership of The Niagara Institute and his time with the World Bank. Terry has a BA (Political Science and Economics) from the University of Toronto and an MBA from Stanford University.