By Brian Taylor, AuD, Editor-at-Large

A few months ago, in the most recent edition of Signal and Noise, I outlined the value of customizing ear coupling by following the advice of Margaret (Margo) Skinner. The basic message was the clinician’s ability to customize earmold plumbing is likely to result in higher levels of patient benefit. Additionally, the ability to customize ear coupling systems is a great way to differentiate your clinic from OTC retailers, who are unequipped to provide patients with a customized earmold.
Now, let’s turn our attention to another facet of the patient-provider interaction that benefits from customization: optimizing gain for the individual wearer.1
To illustrate this point, we will examine the work of another important figure in the history of hearing aid fitting, Denis Byrne, a pioneer in prescriptive gain fitting approaches who died more than 20 years ago. He reminded us that when you are fitting hearing aids if you can’t write down what you’re doing so that others can examine it, you probably shouldn’t be doing it.
First, a brief history
The need to customize gain can be traced back to some controversy, occurring more than 75 years ago. In 1946, there were two dueling approaches to hearing aid fitting and selection. The first approach, originating from the Psycho-Acoustic Laboratory at Harvard University and the Central Institute for the Deaf in St. Louis covered in the so-called Harvard Report, essentially called for a one-size-fits-all approach.
According to Hallowell Davis and his co-authors, regardless of the shape of the audiogram, individuals tend to benefit from the same “flat” hearing aid response with essentially equal amounts of gain across frequencies.

In contrast, others, among them the “father of audiology,” Raymond Carhart, advocated for a fitting method mirroring the audiogram. A more tailored approach in which the amount of gain applied at each frequency was inversely proportional to the degree of hearing loss at each of the frequencies tested. Once commonly referred to as selective amplification, and now known as the prescriptive fitting approach, this method has been used to fit virtually all hearing aids for the past forty years. To learn more about this pivotal time in the early days of audiology, readers are encouraged to find this short piece authored by James Jerger in 2018.
Even though the prescriptive fitting method has won the day, if you spend any time with hearing care professionals (HCPs), either in their clinic or at a conference, many grouse about how “hot” prescriptive gain targets tend to be for their patients. What these HCPs are saying, I think, is that on the day of the fitting patients prefer much less gain than the two most popular prescriptive targets, NAL and DSL, call for, especially for soft high frequency sounds. Therefore, no matter what version of the NAL or DSL target an HCP might use, they end up turning down gain to please the patient and improve immediate acceptance of their hearing aids. As discussed later, hearing aid manufacturers, by building it into their own proprietary prescriptive gain targets, automatically reduce gain, especially for soft sounds.
Is it right or just right-sounding?
Many clinicians, when selecting a prescriptive method in the fitting software of their favorite manufacturer, choose that manufacturer’s proprietary fitting targets. This is a gain and output algorithm that has been created by the manufacturer to work similarly to one of the scientifically derived prescriptive targets. Clinicians who rely on the proprietary targets usually believe it to be a better starting point than the NAL-NL2 or DSL v5.0 because it is presumably better suited to the specific processing of that manufacturer’s devices.
This approach sounds right, but there is no science to back it up. After all, right-sounding is not the same as right.

On the other hand, there is science to support the use of both the NAL-NL2 and DSL v5.0. Since the NAL targets are the most commonly used with adults, let’s explore it further. In 1976, Denis Byrne co-created` the first National Acoustic Laboratories (NAL) prescriptive gain formula. One of two well-known prescriptive gain targets used today (the other being the DSL), validated with thousands of hearing aid wearers. Based on sound scientific principles, both formulas use an iterative process, meaning that as more patient data are collected, their targets change slightly with every new version that is released. Clinicians practicing for many years know, before the NAL-NL1 and NL2, which were designed to work with hearing aids that employ wide dynamic range compression, there was the NAL-R (R = revision) and another NAL modification for severe-profound loss.
Another important aspect of the NAL family of targets that you probably learned in school, is that its main goal is to equalize loudness, which basically means make amplified sound audible and comfortable for the wearer across all frequencies. Since NAL tries to balance comfort and audibility, you can think of NAL’s loud equalization strategy as somewhat of a compromise between the one-size-fits-all, flatter frequency response called for the Harvard Report and Carhart’s original notion of gain mirroring the audiogram. A quote2 from Denis Byrne best illustrates this point:
“NAL research agrees with other recent research in indicating that the optimal frequency response differs from one client to another…..NAL research does show that variations is audiograms require less variation in frequency response than is often supposed and provided in many selection procedures. NAL is, therefore, in a sense, a reconciliation between the apparently conflicting evidence for and against selective amplification.”
-Page 121, Chapter 8, Implications of the NAL Research for Hearing Aid Gain and Frequency Response Selection Strategies. Acoustical Factors Affecting Hearing Aid Performance, 2nd edition, Studebaker and Hochberg, 1993.
There you have it: according to Byrne, the NAL is a compromise between those two dueling approaches mentioned earlier. If the NAL targets are already a reconciliation between these divergent approaches, why do proprietary “first-fit” gain targets found in all hearing aids provide even less gain that what NAL calls for?
Stop me if you’ve heard this before
It’s generally acknowledged that the hearing aid manufacturer’s proprietary first-fit approach yields less gain, especially for soft, high frequency inputs than the NAL-NL2. This difference can be as much as 15 dB for soft, high frequency sounds and this difference holds true even when the clinician selects the “NAL-NL2” method in the manufacturer’s fitting software, as this 2015 study demonstrates.
The prescribed gain difference between the manufacturer’s proprietary first-fit approach and the NAL-NL2 prescriptive method is not necessarily a bad thing. After all, manufacturers produce hearing aids for a worldwide market and many of the people fitting hearing aids in markets outside of North America, Western Europe and Australia/New Zealand oftentimes lack the proper verification equipment. Additionally, in some locales, hearing care professionals might lack the advanced training needed to put modern verification methods into practice and rely on the manufacturer to help get them in the ballpark for gain and output.
It’s important to remember, though, gain differences between a manufacturer’s proprietary first-fit and the NAL-NL2 reflect two opposing goals: One, a manufacturers’ top priority is to serve a global market for hearing devices. It is in their best interest to ensure these devices are fitted as efficiently as possible and once fitted they stay in the wearer’s ears from the get-go. Thus, immediate first-fit acceptance is a primary goal. Two, for scientists, including the late Denis Byrne, their highest priority is optimizing audibility and comfort of speech, using data collected from thousands of individuals to refine their targets.
Of course, these two goals – optimizing audibility and immediate wearer acceptance — often conflict, and it falls on the shoulders of the HCP – who actually fit the hearing aids and must contend with complaints about loudness – to sort them out for each individual fitted in their clinic.
We know most HCPs accept the manufacturer’s proprietary approach to selective amplification and simply trust “first-fit”. Assuming survey data from 2010 is unchanged, most HCPs believe their favorite hearing aid manufacturer’s first-fit algorithm gets them in the ballpark and don’t take the time, either at the initial fitting appointment or during any subsequent follow-up appointment to ensure, through the use of probe microphone measures, that gain targets are a close match of the wearer’s prescribed NAL target.

Considering the 2020 MarkeTrak10 reports indicate overall hearing aid satisfaction is around 85%, an “immediate acceptance” approach might be, in many cases, “good enough” for many wearers. In the end, any hearing aid – even those with gain set well below the NAL targets — is probably better than not wearing any hearing aid at all. Since “good enough” can be obtained with a self-fitting hearing aid or the use of a manufacturer’s first-fit button, clinicians should be motivated to optimize audibility using one of the validated prescriptive approaches.
Here’s the rub: In a world where self-fitting OTC devices soon are likely to be available, it is entirely possible that a patient could become satisfied with “good enough” aided performance without ever experiencing the benefits of optimized gain, a goal that stems from using REM to ensure NAL gain targets have been matched in the clinic. Indeed, the bitter reality is that if you are an HCP who is relying on proprietary “one-click and done” gain targets and not attempting to match the NAL targets, the gain you are providing patients when they walk out of your clinic door could be substantially less than what that same patient would get from self-fitted instruments, purchased over-the-counter.3
Research that supports the use of matching the NAL targets
So, if overall hearing aid satisfaction is above 85% in a world where the majority of clinicians rely on a first-fit approach that undershoots the NAL gain targets for soft sounds, is it even worth the clinician’s time and effort to chase after an additional 5 to 15 dB of gain to more precisely tailor the hearing aid’s response to the individual?
To address this question, let’s examine some research. Here are six studies that support the customization of validated gain targets using real ear measures.
- We know from a 2018 study, conducted at Washington University, that individual soundbooth performance for speech recognition in noise is significantly better for a NAL-NL2 fitting compared to a manufacturer-derived first-fit. In addition, this study had a real-world component in which self-reports of real-world benefit showed significantly better results for the NAL-NL2 fitting for nearly all study participants.
- Using the APHAB, a validated 24-question self-report of benefit, a 2012 study found that when the NAL-NL1 fit was compared to the manufacturer’s fit, there was significantly more benefit for the NAL fitting in real-world use. In addition, this study found 68% of wearers preferred the NAL fit to the manufacturer-derived fit, compelling evidence that matching the NAL yields relatively good first-fit acceptance.4
- A 2016 study, published in Hearing Review took a slightly different approach to addressing the value of customization of audibility. Amlani and colleagues used a 14-item questionnaire that measured attitude and behavior toward perceived value along five dimensions: emotion, perceived quality, price, perceived value, and behavioral intent for three groups of participants. Group 1 were “experienced” wearers who consisted of those with more than one year of hearing aid use experience. Group 2 were “In-the-Drawer” wearers who had previously purchased amplification but did not wear their devices. Group 3 consisted of “first-time” wearers of amplification. Their results demonstrate that REM used to match a prescriptive target reduced emotional distress, and improved perceived quality of service and value of the hearing aid fitting experience compared to the first-fit method in three groups of participants. Perhaps simply taking the time to conduct REM is enough to demonstrate to patients the value of the clinician and her ability to carefully match a scientifically derived target
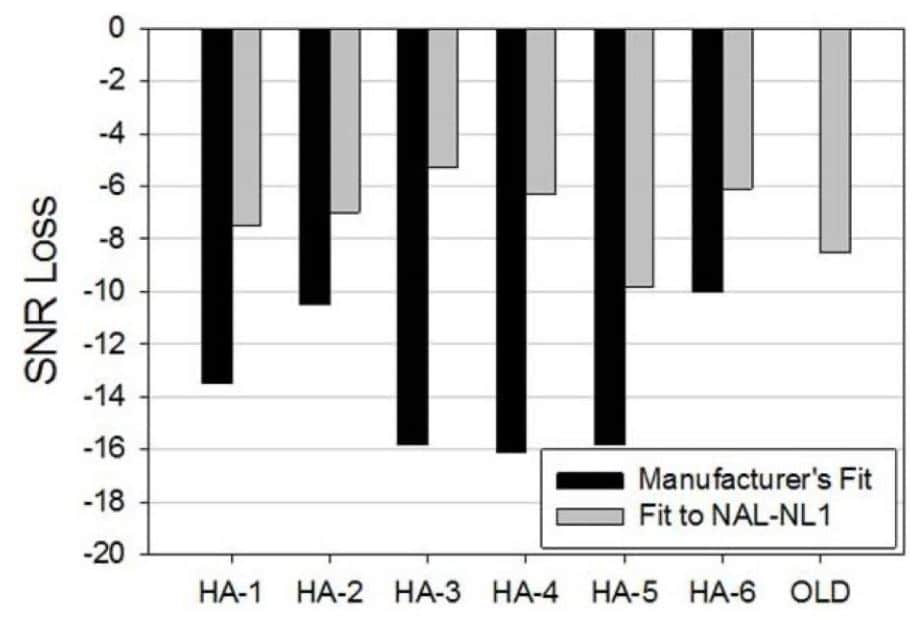
- Perhaps the most persuasive evidence that matching a validated gain target translates into improved speech intelligibility comes from the work of Ron Leavitt and Carol Flexer, summarized in this 2021 20Q article. In a couple of different articles, Leavitt and Flexer compared aided Quick SIN scores for the same hearing aid but fitted with two different prescriptive methods. As shown in Figure 1, initially, when the hearing aids were fitted to the manufacturer’s proprietary first fit, aided Quick SIN performance was relatively poor, but when the same hearing aids were re-fitted to more closely match the NAL target, performance in noise improved upwards of 10 to 12 dB. By simply taking the time to optimize audibility by relying on a validated prescriptive target and confirming it with REM, a hearing aid performing poorly in background noise was transformed into one that performed well in noise – with just a few clicks of a mouse.5
- While you’re on the Audiology Online website reading Ron Leavitt’s 20Q, you might want to go back one month to the June 20Q and read Anu Sharma’s hypothesis about the possible neuroplastic effects of under-fitted hearing aids. In that article, she mentions a study in which underfit hearing aid wearers (presumably from clinicians who rely on first-fit, immediate acceptance methods) showed a lack of neuroplastic changes in the auditory cortex from amplification even after extended periods of hearing aid use. This is a finding that needs additional data to confirm, but one worthy of our attention.
- Finally, one recent meta-analysis confirms that optimizing audibility leads to a bounty of positive outcomes. Self-reported listening ability, speech intelligibility in both quiet and noise, sound quality and wearer preference favored a fitting that optimized audibility compared to an out-of-the box and onto-the-ear first-fit approach.
Standing apart from OTC
Audiologists and hearing instrument specialists, armed with their trusty probe microphone system used to match a validated prescriptive target, are better equipped than either a hearing aid manufacturer or self-fitting algorithms to optimize audibility. So, let’s jump in a time machine and visit a future where OTC hearing devices are regulated and available in a variety of places.
What can clinicians do to stand apart from hearing aids purchased over-the-counter?
The simple answer, of course, is to customize as many elements of the assessment and treatment process as possible. Let’s look at how customizing gain within 3 to 5 dB of the validated NAL (or DSL) targets for the individual wearer can differentiate you from OTC retailers.
First, you must have confidence that when the occasional patient grumbles about their new hearing aids being too loud, sharp or tinny, optimizing audibility and comfort of soft, average and loud sounds by closely matching the NAL prescription as a starting point remains a wise strategy. In fact, this 2010 Western University study, which used the DSL v5.0, known to provide slightly more gain than the NAL-NL2, was shown to approximate the preferred listening levels of study participants within 2.6 dB, on average, of 60 dBA running speech. In this study, 30 adults with varying degrees of hearing loss and audiogram configurations were fitted to the DSL targets, seen for follow-up at 30 days where fine-tuning was completed if necessary, to adjust the devices to the participant’s loudness preferences. Following any fine-tuning at this follow-up visit, participants wore their devices another 60 days to allow further acclimatization over a total of 90 days. At the end of 90 days, their preferred listening levels were measured and found to be a close approximation of what the DSL target called for.

To support the use of the NAL and allowing wearers ample time to acclimate to it, look no further than the handful of studies evaluating trainable hearing aids. In one 2012 study , archived at the Signia professional library using some of the first trainable hearing aids, Catherine Palmer found that when a group of 35 new wearers were fitted to the NAL-NL1, after as much of two months of training, on average, gain was only trained down 2-3 dB. In another 2013 study using trainable hearing aids, the researchers found that for a group of experienced wearers, on average, gain was only trained down 1-2 dB across five different listening situations. These results suggest wearers tend to end up with gain similar to where they started, so why not start where audibility is optimized?
Second, a handful of patients are likely to still grouse about some sounds being too sharp, tinny or loud. (By the way, occasional patient grousing is expected and okay – it’s our job to listen!) That’s when your counseling skills must shine. When you tell patients, it takes time to reacclimate to sounds they have missed for many years, they tend to follow the advice of the trusted professional. Thirty years ago, when many peak clipping hearing aids, arguably, were not very good, there were several articles written about how to counsel patients through this acclimation process. Mead Killion even created an alter ego, Dr Abonso, an acronym that stood for Automatic Brain-Operated Noise Suppressor Option. Dr. Abonso gave several talks and wrote a few articles that discussed HABRAT: Hearing Aid Brain Rewiring Accommodation Time. Likewise, a 2001 Seminars in Hearing article, written by Gus Mueller and Tom Powers stated that, “you have to hear what to don’t want to hear to know that you don’t want to hear it.” Solid advice for anyone fitting hearing aids – then and now! Today, even though hearing aid processing is more sophisticated, it would be prudent for HCPs to hone their counseling skills around
HABRAT, especially if they want to optimize the individual’s audibility by using the NAL targets. The alternative to this counseling approach, incidentally, is to turn down gain, shortchange the patient of many important speech cues for soft and average inputs, but reduce the chances of complaints.6

Third, conduct probe microphone measures per best practice guidelines, matching target gain for soft, average and loud sounds within +/- 3 to 5 dB across frequency. To add a level of precision to target matching, consider using the 2007 British Society of Audiology guidelines that suggest getting within 5 dB of the NAL target from 250 to 2000 Hz and 8 dB of the target at 3000 to 4000 Hz. To speed the process, use your favorite manufacturer’s version of autoREMfit, a procedure proven to be reliable and accurate.
Fourth, remember prescribed gain targets represent an average. Research shows that about an equal number of wearers prefer gain either just below or above the average starting point. For example, a recent study using a prototype self-fitting hearing aid showed that 68% of study participants self-adjusted to within +/- 5 dB of the NAL-prescribed target for average level, high frequency inputs. Even though most wearers, given ample time and counseling, will acclimate to a well-matched NAL prescribed gain starting point, it is impossible to predict who might prefer large deviations from that target. Therefore, it is useful to provide wearers, at least those who are willing to try it, with the ability to make manual adjustments. Recent advances in deep learning and live neural networks, such as what’s found in the pioneering feature, Signia Assistant, enable wearers to make even more precise adjustments in real time using their smartphone.
Finally, in a world where a person who purchases self-fitting hearing aids over-the-counter is likely to achieve a “good enough” fit on their own, there will be plenty of opportunities to take these ordinary fittings and make them extraordinary be following the basic principles, pioneered by Denis Byrne, in your clinic.
Footnotes:
- The term “optimizing gain” is used throughout this article. Perhaps a better term would be “optimizing audibility” or “maximizing effective audibility.”
- If you are looking for more memorable Denis Byrne quotes (and who wouldn’t?) this 2015 20Q from Gus Mueller has what you want.
- Two recent peer reviewed studies indicate that many wearers can get within +/- 5 dB of the validated NAL target for average level inputs when the wearer is trained to use a simple smartphone-based interface. Interestingly, neither of these studies reported findings for gain for soft inputs using a self-adjusted control. Study one is here. Study two can be found here. Interestingly, the ability of the wearer to achieve adequate gain for soft sounds may be one of the leading factors associated with successful hearing aid use, so says this 2014 study.
- Although these two studies, Valente et al, 2018 and Abrams et al 2012, offer compelling evidence that using REM to individualize validated gain targets leads to better wearer outcomes, this 2021 evidence-based review serves as a bit of a reality check. Their meta-analysis suggests that while REMs might improve outcomes statistically, this conclusion is based on a small number of studies with a limited number of participants. Also, given the time it takes to conduct REM during a 60-minute appointment, the authors highlight the need for studies that evaluate the cost-effectiveness of REM
- In Leavitt’s July 2021 20Q article, he mentions that nearly all patients in his study were routinely underfitted in the high frequencies by 10 to 17 dB, relative to the NAL target. Oftentimes they were under-fitted in the highs by as much as 30 dB. Amazingly, the average hearing loss of the 97 participants in this study had a pure tone average of 50dB with a gently sloping configuration. Given the mild nature of these hearing losses, we can surmise that many of these patients initially had little to no high frequency gain – and all patients were originally fitted by a licensed professional. It is safe to say these under-fits are not too different than what we would expect from self-fitting devices sold OTC.
- Most manufacturers, including Signia offer automatic acclimatization features in their fitting software which can provide a compromise if a patient does not acquiesce to your counseling; a far better alternative than shortchanging audibility.
About the Author
Brian Taylor, AuD, is the senior director of audiology for Signia. He is also the editor of Audiology Practices, a quarterly journal of the Academy of Doctors of Audiology, editor-at-large for Hearing Health and Technology Matters and adjunct instructor at the University of Wisconsin.
*feature image courtesy of Cambridge in Color