Today’s post continues a Shingles series that started with an obscure link to Red Ear Syndrome. That link lead to posts on shingles in general and shingles in the ear. The latter co-mingles with the specifically-named Ramsey-Hunt syndrome, pictured horrifically above, the subject of the next several posts in this series.
RHS is a Confusing Bundle of Syndromes
Despite a specific-sound name, Ramsay Hunt Syndrome (RHS) is a nebulous term that causes diagnostic irritability (e.g., authors of “Ramsay Hunt Syndrome: To Bury or to Praise” voted to bury it!). That’s because RHS covers totally separate neurological syndromes bunched together for no good reason other than they were discovered by the eminent 20th century neurologist Dr. James Ramsay Hunt (1872-1937). Too bad for Dr. Hunt, who seems to have been a good guy, to be remembered chiefly for a horribly painful condition and for totally confusing the medical literature.
Three syndromes comprise RHS:
- Ramsay Hunt type 1: “rare, degenerative, neurological disorder characterized by myoclonus epilepsy, intention tremor, progressive ataxia and occasionally cognitive impairment .” NOT in Audiology’s Scope of Practice.
- Ramsay Hunt type 3: “occupationally induced neuropathy of the deep palmar branch of the ulnar nerve… also called Artisan’s palsy.” This type is so obscure that it doesn’t even have it’s own write-up on Wikipedia and Artisan’s palsy is not a valid Scrabble word. Way outside our Scope of Practice.
- Ramsay Hunt type 2: Herpes zoster oticus. This is the one for which Dr Ramsay Hunt is famous and the one that has to do with Audiology. RHS/2 is the “reactivation syndrome of herpes zoster in the geniculate ganglion. It has variable presentation which may include Bell’s palsy, deafness, vertigo, and pain.”
What’s the Geniculate Ganglion?

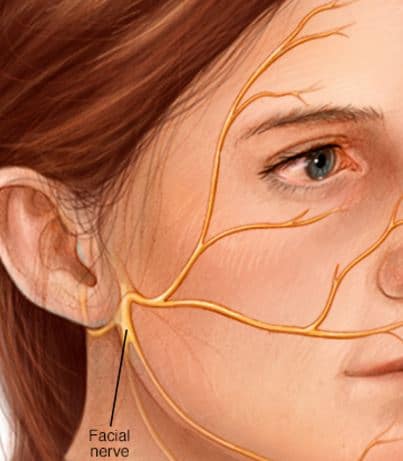
Figure 1. Auditory nerve, vestibular nerve, and facial nerve Bunched Together to Enter and Exit the brainstem. Facial Nerve branch enters from the geniculate body.
Readers who’ve been following this series are right to ask, since that anatomical term didn’t surface in previous discussion of shingles, the ear, or the ear-brain neural connections. Figure 1 illustrates all that’s packed into the internal auditory canal, which is a lot.
The geniculate ganglion sits up at a fork in the road in Figure 1, where the nerves enter or leave the brain on their way to and from the ear. It’s the same bottleneck where all our vestibulocochlear nerve problems seem to hang out. What a mess.
The facial nerve (CVII) sends a sensorimotor branch down through the canal, sandwiched in with the hearing and balance nerves and blood supply to the inner ear. The intersection for that branch and others on the Facial nerve is the geniculate body, which serves as central headquarters for facial muscle movement, touch sensation in the ear canal and parts of outer ear, taste on much of the tongue, and eye and mouth moisturizing.
So many things in such a tiny area — so many ways to go wrong.
Ramsay Hunt Type 2 (RHS/2): With Herpes Zoster Oticus Most of the Time
In RHS/2, the varicella zoster virus lives in the geniculate body and becomes RHS/2 upon re-awakening — “following” the facial nerve. The vestibulocochlear nerve is in such close proximity to the geniculate ganglion that it’s usually affected as well. The strict definition of the RHS Type 2 is “peripheral facial nerve palsy accompanied by an erythematous vesicular rash on the ear (zoster oticus) or in the mouth” (more on that in the next post).
Right away, you can see the confusion: strictly speaking, you can have RHS/2 without any signs in the ear, in which case it’s RHS/2 without herpes zoster oticus. Confusing. But most of the time the ear’s involved so herpes zoster oticus is frequently referred to simply as Ramsay Hunt.
RHS/2 often begins with paroxysmal (sudden, stabbing) pain deep in the ear that moves out to the pinna and transitions to a constant, dull and diffuse pain within several days. From start to finish, all sorts of symptoms are possible, though not all symptoms happen to everyone affected:
- Painful rash
- ear, ear canal, ear drum
- lower face
- mouth: hard palate, tongue
- neck, and/or scalp
- Intense ear pain
- Unilateral hearing loss
- Unilateral hyperacusis (increased sensitivity to loud sounds) due to paralysis of the stapedius and tensor tympani muscles of the ear
- Nystagmus (eyes twitch back and forth or up and down in tandem)
- Vertigo
- Vomiting
- Tinnitus
- Acute facial nerve paralysis or facial weakness
- Loss of taste in front 2/3’s of the tongue
- Dry mouth
- Dry eyes
- Malaise
- Fever
With that many symptoms manifesting in a variety of ways, it is no wonder that diagnosing RHS/2 can be problematic. The diagnosis is even more challenging when there is no rash present (yes, that can happen). In that case, Bell’s palsy and RHS/2 are hard to tell apart, but it is important to do so. Next post in this series will look at the rash and continue the Ramsay Hunt story.
References
References are accessible by clicking on the links in the post. The following reference was used for general information scattered throughout the post:
Sartoretti-Schefera S, et al. Ramsay Hunt Syndrome Associated with Brain Stem Enhancement. AJNR 1999 20: 278-280.
feature image from Mayo Clinic






Thank you for reporting this! As someone currently suffering from this syndrome, I can’t begin to tell you how refreshing it is to read something about it that makes it easy to understand.