by Eugene R. Worth, MD

Eugene Worth, MD
Now that you understand about ear barotrauma and other ear or sinus pathology and SCUBA diving from my previous post, let’s see if we can put it all together – ear pathology and diving.
Of course, I have a case to discuss. By the way, all of the cases presented here are real. I have carefully hidden where and when these cases happened. Please do not assume that they all occurred in Southern Utah.
The Case Of The Painful Palate
This is a 29 y/o woman who was on a live-aboard trip out of San Diego, California. Live-aboard trips in SCUBA are much like any other cruise, except the accommodations are not quite as nice. That said, you get to dive 4 or 5 times per day, and every dive is in a new location. Most live-aboard cruises allow divers access to some of the most remote locations in the world. Some of the cruises are 1 to 2 days away from medical care, but that is a different story.
This woman complained of difficulty clearing her ears on every dive. By the end of Day 3 of diving, she complained of pain in her palate. In fact, with every dive it got better at pressure then got worse after she got back on the boat. She is an EMT at a hospital and was diving with three physicians on the boat. (Hint – therein lies part of the problem in this case.
 By Day 4 of the trip, she approached one of the physicians about her problems. She was already taking pseudoephedrine. The physician was convinced that she had a sinus infection, so he gave her an injection of Bicillin. Strange choice of antibiotic, but he had it in his travel bag. For those of you so inclined, Bicillin used to be the treatment of choice for acute syphilis. It has never been the drug of choice for an acute sinusitis. Needless to say, she had a sore bottom but no relief of her symptoms. Thankfully another physician had a Z-pack (azithromycin) with him. While it is a better choice of antibiotic for acute sinusitis, it did nothing for her symptoms.
By Day 4 of the trip, she approached one of the physicians about her problems. She was already taking pseudoephedrine. The physician was convinced that she had a sinus infection, so he gave her an injection of Bicillin. Strange choice of antibiotic, but he had it in his travel bag. For those of you so inclined, Bicillin used to be the treatment of choice for acute syphilis. It has never been the drug of choice for an acute sinusitis. Needless to say, she had a sore bottom but no relief of her symptoms. Thankfully another physician had a Z-pack (azithromycin) with him. While it is a better choice of antibiotic for acute sinusitis, it did nothing for her symptoms.
Along comes the third physician. By this time, they are completely confused. He thought that she had decompression illness. No consultation by the nearest diving medicine physician, but he did call the airline and arrange for oxygen to be provided to this young woman for her flight home. One of the premier training programs in undersea and hyperbaric medicine is located in San Diego. In fact, if you call Divers Alert Network (DAN) with a diving medicine problem, you will likely speak with one of the UCSD diving medicine physicians. They are highly recognized, and one of them has written a prized textbook on the subject.
She returned to town on a Friday, then she reported to work in the emergency room on Saturday morning. She related the symptoms to the ER (Emergency Room) physician on call. He is not a diver and not a specialist in undersea medicine. He wrote her a prescription for a Medrol Dosepack.
So far, what do we know? We know that she has terrible palate pain bilaterally that is worse at sea level and better at pressure. We know that she had difficulty with ear clearing on every one of her dives during the trip, but she was able to clear and did not change the dive profile based on her ears. Finally, we know that she didn’t have syphilis, unlikely that she had a sinus infection (more to come on this), and she may/may not have decompression illness.
Aside: It’s My Weekend Off
This woman decided to speak with the hyperbaric physician at the hospital. On that particular weekend, I was off call and had gone out of town to our cabin in the mountains. It’s about an hour from the hospital at 8000 feet elevation. It was a beautiful fall weekend, and the leaves were turning colors. It was also one of the last weekends that I could get paint on the exterior of the cabin in preparation for winter.
The hyperbaric physician that weekend was someone trained in hyperbaric medicine but with no experience in undersea medicine. He was a brilliant and resourceful physician and one of the hospital’s intensive medicine physicians. She approached him with her story. After due consideration, he knew that one of the oral surgeons was making rounds and consulted him. This resulted in a Panorex X-ray to rule out dental pathology. There was none. Based on that, our ICU (Intensive Care Unit) physician ordered a CT (computed tomography) of the sinuses looking for sinusitis or other sinus/facial pathology. There was none. He had examined her ears and did note fluid and bubbles behind both tympanic membranes. She had some dullness in her gross hearing and felt her ears “gurgle” when she bent over. Hmmmm. Now what to do?
About 2PM on Saturday afternoon, he got another diving medicine call. There was a young man who was diving at Flaming Gorge in Utah. Although he did not have a provocative dive history, he had some shoulder pain that was worse when crossing an 8000 foot mountain pass on his way home. This is when the weekend physician called me. He was too deep (so to speak) in diving medicine questions to adequately cover the hyperbaric chamber. Needless to say, after hearing about both cases, I cleaned up the paint brushes, we packed the car, and we drove back home so I could finish my weekend off working at the hospital.
Back to the Painful Palate
At first, I had a brief opportunity to talk with the young woman before the Flaming Gorge diver arrived. I was also able to review what had happened to her and the tests that had been performed. There was no visible pathology and all tests were negative. At this point, she was badgering me to put her in the chamber to treat her decompression illness. After all, I was going to put the other diver in the chamber for exactly that reason. This was becoming a real dilemma.
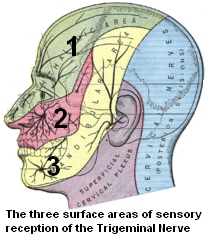
Figure 1. Surface areas of sensory reception of the Trigeminal (N5) nerve.
However, I performed a more thorough physical examination. She had no other evidence of decompression illness than an exquisitely painful palate. She also related to me that for the past several days, her taste was suddenly “off.” I found some mild numbness on the side of her face that corresponded to the maxillary branch of cranial nerve 5 (Figure 1, area 2). Here is the dilemma; do I put her into the hyperbaric chamber and treat her for something she probably doesn’t have?
No, I elected not to treat her. There is another definitely plausible reason for her to have these symptoms. I called one of my ENT (Ear, Nose, and Throat) friends and asked if she could come to his office on Monday for evaluation. I told him what I thought she had. Meanwhile, she should continue the oral corticosteroids.
ENT Exam
Indeed, she had numbness over the maxillary area of CN5. If you are an anatomy buff, this is known as the V2 area. (V is the Roman numeral for 5.) As we review the course of V2 (the maxillary nerve), there are several areas where V2 passes through narrow bony canals. One of these areas is in close proximity to the roof of the maxillary sinus. Any excess pressure in the maxillary sinus can press on V2 and cause it to become swollen and inflamed. Since V2 is a purely sensory nerve, the only deficit noted when this nerve is inflamed is pain sensation. Following V2 to its endpoint, we note that the alveolar nerves (for the maxillary teeth) are innervated by end branches of V2. Interestingly, the hard palate is innervated by the greater palatine nerve, another end branch of V2.
Our ENT surgeon performed a careful otological examination, complete with tympanometry and audiometry. These were consistent with her failure to equalize and thought to be temporary once the pressure insults were stopped. In addition, he noted that he could clearly see the chorda tympani behind pars flaccida of the tympanic membrane bilaterally.
Why Is The Pain Better At Pressure?
Several logical questions would be, “Why is the pain better at pressure? And, why is it worse after surfacing? Isn’t that decompression illness?”
There are some other tidbits of information that you need to know in order to solve this dilemma. First, the physical law that affects body fat underwater. Body fat is compressible to a small but measurable degree. No matter how tightly you adjust the buoyancy compensation device (BCD) to your body on the boat, once reaching 2 atmospheres of pressure (or greater), the BCD is loose and needs to be re-adjusted. Nerve tissue has a significant amount of fat in the perineural cells, thus nerves are also compressible with increasing atmospheric pressure.
Think again. Why is her pain better (nearly gone) under pressure? The swelling of the nerve is reduced, thus relieving the pain as the nerve courses through the bony canals. While putting her in the hyperbaric chamber would have relieved her pain, it does so by compressing the nerve. Pain relief would be temporary and might lead to the conclusion that she had decompression illness when she, in fact, did not. Her pain is the result of swelling, thus leading to inflammation of the nerve in its bony canal. The solution is to reduce the inflammation of the nerve. These are the hallmarks of V2 Syndrome.
Can We Solve The Problem With Her Taste?
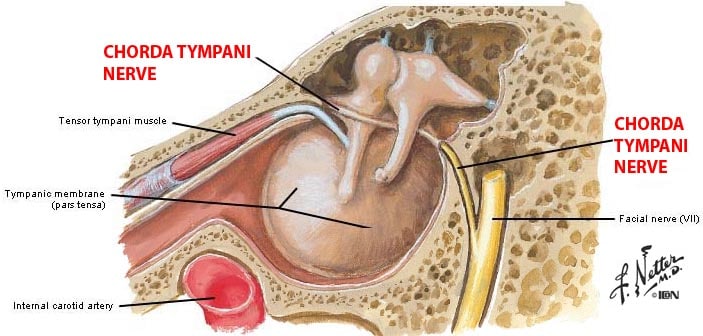
Figure 2. Chorda tympani nerve location relative to the middle ear. (Netter illustration).
The chorda tympani nerve is rarely visible on ear examination. When it is visible, the cause is almost always secondary to ear barotrauma. The chorda tympani nerve is a branch of CN7, the facial nerve. The facial nerve is nearly all muscular and very little sensory. The chorda tympani nerve is a sensory branch of the facial nerve and travels through the roof of the middle ear cavity on its way to … wait … wait for it … innervating the taste buds on the anterior 2/3 of the tongue (Figure 2).
Lessons Learned
Most physicians fail to spend the time or effort to listen to the patients. With careful questioning, most patients will tell you their story. With enough inquisitiveness and background information, the disease process will reveal itself and treatment options can be formed on a scientific basis. Hence the solution for this problem diver. The primary problem was ear barotrauma. The more vigorously she tried to clear her ears, the more she compounded her symptoms.
Decompression illness can be elusive. That said, it is extremely rare that decompression illness have its only complaints in the face and sinuses.
Yes, I lost a weekend off. However, undersea medicine is not what one practices exclusively when living in a desert at higher altitude. It can be rewarding and a great deal of fun. This case was challenging but interesting. And, yes, the diver from Flaming Gorge did well.
Fat compresses under pressure. Nerves have a significant amount of fat. Therefore, the nerve will compress (decreasing the evidence of inflammation) under pressure.
This caveat is one to always remember: Doctors who SCUBA dive are not diving doctors! There is a reason for a diving medicine specialty. This woman had a number of needless negative tests. Those include several rounds of antibiotics, a Panorex X-ray, CT of the sinuses, and nearly a decompression illness hyperbaric medicine treatment.
Treatment and Resolution
The emergency room physician on staff that day was known as an “ER cowboy.” “Never mind facts, full speed ahead” would be a good motto. Another might be, “Ready … Shoot … Aim.”
For all the wrong reasons, he got the treatment right. This woman was much relieved within two days of starting nasal decongestants and a Medrol Dosepack of high dose corticosteroids.
For the ER physician, I give him credit. Without full knowledge, the treatment recommended just happened to work.
Dr. Eugene Worth is the Medical Director for Hyperbaric Medicine at Dixie Regional Medical Center in St George, Utah. Dr. Worth received his MD degree from the University of Missouri-Columbia, in Columbia Missouri. He then completed his internship and residency in Anesthesiology at the University of Missouri-Columbia Hospital and Clinics. Dr. Worth is a board-certified Anesthesiologist with 13+ years in private and academic practices. His subspecialty area was cardiac and major vascular anesthesia including heart transplantation. He has received many honors and awards for his work, and he is a prolific researcher and author. He has practiced wound care and hyperbaric medicine since 2002. The latter is of special interest because this sub-specialty, where he is certified in Undersea and Hyperbaric Medicine, often leads him to engage in underwater research. And, much of what he sees and treats relates to middle ear and Eustachian tube disorders. He is a recreational diver and a NOAA (National Oceanic and Atmospheric Administration) Diving Medical Officer.








A brilliant write up, bringing to light the fact that increased pressure (barometric) on an inflamed nerve could actually reduce the pain. May be noticed during swimming with a ruptured spinal disc pressurizing the sciatic nerve ! The pain reduces temporarily only to return when out of the water.