Many hearing professionals have expressed concerns that OTC hearing aid sales will result in dissatisfied users because:
- The instruments are not professionally fitted
- An audiogram is necessary
- OTC-sold devices (previously defined as PSAPs) are of poor quality and will not meet the needs of the hearing impaired, and
- Poor experiences by the purchaser will discourage them from seeking additional assistance and purchasing a “real” hearing aid
- A universal, basic hearing aid cannot manage all hearing losses
The objection that hearing aids are not fitted professionally in an OTC model was discussed in a previous post.
OTC Hearing Aid Fittings – Importance of the Pure-Tone Audiogram
Hearing professionals have expressed the importance of recording a person’s hearing loss via an audiogram. This is cited as being necessary for the proper fitting of hearing aids, and that without the audiogram, appropriate hearing aid fittings are unlikely to occur – that a good audiogram is mandatory.
The Necessity of the Audiogram
What defines hearing loss? Is it some arbitrarily-determined hearing loss identification based on a dB level or range, or is it based on the consumer’s self-perception of hearing loss? These are likely to be very different descriptions of hearing loss, leading to different actions taken and accepted by the consumer (the person making the ultimate decision). Perhaps the concept of accepting hearing levels as a litmus test for hearing aid use should be applied with greater reservations than currently suggested.
It is important to understand that hearing aids are not purchased based on an arbitrarily-determined degree of hearing loss. How often does a person visit a hearing professional and indicate they want to purchase a hearing aid because they have a 35 dB average pure-tone hearing level? In reality, hearing aids are purchased and worn based on the degree of “hurt,” not on the measured hearing level. If the “hurt” is not great enough psychologically, emotionallly, socially, or economically to the consumer, there may be no “hearing loss” as far as consumers are concerned, and seldom will attempts to convince them otherwise succeed. This may have entered into the results of a study of 76 individuals having significant hearing loss and advised to pursue use of a hearing aid by an audiologist. Of the 76, 26 choose not to pursue hearing aids, 24 opted to purchase, but soon rejected, and 26 pursued hearing aids and were still wearing them 6 months later1.
With respect to the audiogram and audiometric thresholds, reports have described not only the variability of audiometric threshold measurements2, but also the questionability of these measurements being used for suprathreshold hearing aid fittings.3,4
That the pure-tone air-conduction audiogram is necessary for hearing aid fittings is questionable, and includes the following reasons:
- Range of Acceptable Thresholds
The audiogram is a gross measurement of hearing sensitivity. It is subject to ±5 dB variability, meaning that it can be off 10 dB at one test frequency to a repeat of that same test frequency. Factually, test thresholds are accepted if there is 10 dB difference between results, and are not considered a real difference until there is a variation of 15 dB or more from one test to another at a given frequency.
- Use of Threshold Data to Program Hearing Aids
Use of threshold data is used to program most hearing aid target gains, and a fundamental assumption in the professional fitting of hearing aids is that the gain-frequency response of the instrument needs to be individualized to the patient’s hearing loss. To this effect, various prescriptive formulae have been proposed to derive amplification targets based on audiometric threshold. 5,6,7,8
Adding the variability of pure-tone threshold data to the range of differences in the fitting target algorithms used by various manufacturers is cause for questioning what all this means (Figure 1). This figure shows the variabiity of target gains of four premium hearing aids (targets up to 30 dB difference). Which is correct? Or as Staab wrote, “whatever you hit is the target9.” The pure-tone threshold was the same for all these formulae to program the hearing aids.
3. Is there actually an “optimal” fitting?
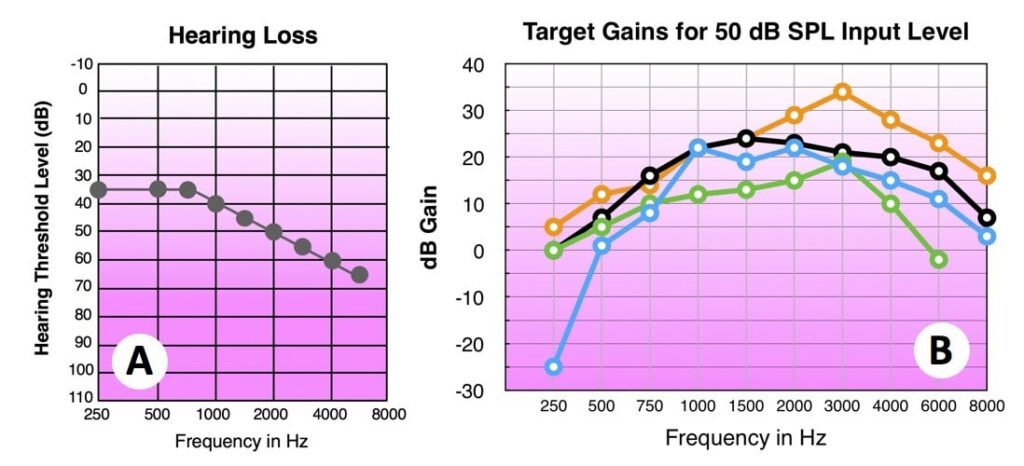
Figures 1A-1B. Moderate sloping hearing loss (A) to which four premium RIC hearing aids were programmed (B). The 2cc coupler responses for the quick fit show that the fitting algorithms for all four are significantly different.9
Hearing Professionals’ Comments About the Audiogram and Hearing Aid Fittings
In a summary of a review of audiometric considerations for hearing aid fitting and success, Bentler states:
“It appears that the more traditional audiometric information such as thresholds, including degree and configuration of hearing loss, speech perception, and loudness ratings are of limited use in predicting hearing aid success, even when broadly defining success. It is clear that the greater the hearing loss, the more the use time of the amplification scheme. It is also clear from this review that other variables or factors account for the positive self-reported outcomes.”10
In a study designed to explore the relationship between pure-tone thresholds, word recognition, and self-reported hearing handicap, poor and variable correlations between the pure-tone threshold (0.37 to 0.73), and word recognition (-0.12 to -0.73) were found to self-reported hearing handicap.11 Since then, much research has focused primarily on the relationship between objective and subjective measures of hearing aid success, but similar relationships continue.
A close approximation of aided performance to prescriptive gain targets (based on audiometric thresholds) is generally assumed to be important for successful and beneficial hearing aid use. This concept has made its way into Best Practices. However, several investigators have questioned the necessity of matching prescriptive gains based on pure-tone thresholds to target gains12,13,14,15, where insignificant differences in speech recognition are obtained when using different formulas. Walden et. al. compared custom versus fixed-format hearing aids and questioned the precise matching of measured to prescribed targets16. Based on their results, they stated:
“…as long as comparable spectral regions are made sufficienty audible and uncomfortable loudness is avoided, there may be a relatively broad range of frequency-gain responses that will suffice.”
This seems to sound somewhat similar to the Harvard Report17 which concluded that a 6-dB/octave rising response was adequate for most individuals.
First Fit
Hearing instrument manufacturers’ first-fit algorithms are known to deviate significantly from actual prescriptive targets.18 Aazh and Moore found that using first-fit, 64% of hearing instruments failed to come within +/- 10 dB of target at one or more frequencies. Similar results were found for open-fit hearing aids.19
An online survey reported that 70% of responding audiologists use the “quick” or “first” fit called up by the fitting software, based on pure-tone thresholds.20 If that is the case, then are we to assume this to be “optimal” fitting? If so, in Figure 1, which target is the right one? Is 30 dB variability from one fitting formula to the other acceptable as hitting the target and providing optimal amplification? And, what if the 10 or possibly 15 dB error of the pure-tone threshold measurement is added in, widening the error even further than 30 dB?
If it is believed that the ear(s) adjust(s) to these target errors over time (brain plasticity), then one might conclude that a wide range of available gain/response configurations might work just as well. It is interesting when fitting hearing aids having multiple environmental listening options, and the consumer is asked to let the dispenser know which is best and whether they sound different, many report that they all (3, 4, 6, or whatever environmental programs exist in the programmed hearing aid), it is commonly said that “they all sound the same.” An exception occurs when low-frequency gain is reduced (often the listening in noise setting), where it is noticed primarily as a reduction in loudness.
Studies have shown that many people do not wear hearing aids at target gain based on pure-tone audiometric thresholds. And if the target gains are reached, there is no greater guarantee of satisfaction with their fittings. If hitting the target resulted in an optimal fitting, “fitting Wizards” would not be needed in programming software.
Hearing Professionals Rank Significant Criteria for Hearing Aid Success
A 3-round Delphi survey of 29 UK hearing professionals was undertaken to identify a consensus on the criteria for hearing aid candidature and clinical practice in fitting hearing aids, specifically for mild hearing loss with and without tinnitus. The Delphi technique is a systematic methodology that seeks consensus among experts through consultation using a series of iterative questionnaires. For patients with mild hearing loss, the greatest priority was given by clinicians to patient-centered criteria for fitting hearing aids: hearing difficulties, motivation to wear hearing aids, and impact of hearing loss on quality of life (chosen as top five by at least 64% of panelists). Objective measures were given a lower priority: degree of hearing loss and shape of the audiogram (chosen as top five by less than half of panelists).21
Summary
How critical is the audiogram to a successful hearing aid fitting? Research does not appear to suggest that is mandatory for this purpose. However, audiometric measurements of various types continue to play an important for differential diagnosis of hearing problems and in counseling consumers.
References
- Humes LE. (2003). Modeling and predicting hearing aid outcome. Trends in Amplification 7: 41–75.
- Staab W.J. (2011). Wayne’s world hearing threshold challenge, Hearing Health and Technology Matters, April 6, 2011. https://hearinghealthmatters.org/waynesworld/2011/hearing-threshold-challenge/.
- Schweitzer H.C., and Donnelly R.C. (2013). Why it’s time to retire the audiogram (for hearing aid fittings). Hearing Health and Technology Matters, June 26, 2013. https://hearinghealthmatters.org/hearingviews/2013/why-its-time-to-retire-the-audiogram-for-hearing-aid-fittings/
- Schweitzer H.C. (2017). All ears are ‘real ears,’ but that’s not enough! Hearing Health and Technology Matters. January 10, 2017. https://hearinghealthmatters.org/waynesworld/2017/all-ears-are-real-ears-but-thats-not-enough/
- Byrne D, Dillon H. (1986). The National Acoustic Laboratories’ (NAL) new procedure for selecting the gain and frequency response of a hearing aid. Ear and Hear 7:257-265.
- Killion M. (1994). Fig6: Hearing Aid Fitting Protocol. Operating Manual. Elk Grove Village, IL: Etymotic Research.
- Cox RM. (1995). Using loudness data for hearing aid selection: the IHAFF approach. Hear Jour 48(2)10:39-44.
- Seewald R, Cornelisse L, Ramji K, Sinclair S, Moodie K, Jamieson D. (1996). DSL: v4.0 for Windows: A Software Implementation of the Desired Sensation Level (DSL[i/o]) Method for Fitting Linear Gain and Wide-Dynamic Range Compression Hearing Instruments. Ontario: Hearing Healthcare Research Unit.
- Staab WJ. (2016). Whatever you hit is the target. Review, May.
- Bentler RA. (2006). Audiometric considerations for hearing aid fitting (and success). Hearing Care for Adults, Phonak International Conference, Chicago, 2006, pp 89-95.
- Giolas TG. 1982. Hearing handicapped adults. Englewood Cliffs, NJ: Prentice Hall.
- Dirks D. (1982). Comments regarding “speech discrimination abiity in the hearing-impaired,” The Vanderbilt Hearing Aid Report, Studebaker G. and Bess F (eds), Monographs in Contemporary Audiology, pages 44-50.
- Humes L. (1986) An evaluation of several rationales for selecting hearing aid gain. J Speech Hear Disord 51:272-281.
- Sullivan JA, Levitt H, Hwang J-Y,Hennessey A-M.(1988) An experimental comparison of four hearing aid prescription methods. Ear Hear 9:22-32.
- Humes L, Hackett T. (1990). Comparison of frequency response and aided speech-recognition performance for hearing aids selected by three different prescriptive methods. JAm Acad Audiol1:101-108.
- Walden T, Walden B, Cord T. (2002) Performance of custom-fit versus fixed-format hearing aids for precipitously sloping high-frequency hearing loss. J Am Acad Audiol 13:356-366.
- Davis H, Stevens SS, Nichols RH, Hudgins CV, Peterson GE, Marquis RJ, Ross DA. (1947). Hearing aids: An experimental study of design objectives. Cambridge, MA: Harvard University Press.
- Azah H. and Moore BCJ. (2007). The value of routine real ear measurement of the gain of digital hearing aids. Journal of the American Academy of Audiology, 18(8), 653-664.
- Azah H, Moore BC, & Prasher D. (2012). The accuracy of matching target insertion gains with open-fit hearing aids. American Journal of Audiology, 21:175-180.
- Beyer C. (2011). Common mistakes in routine hearing aid fitting. https://www.audiologyonline.com/ask-the-experts/common-mistakes-in-routine-hearing-39.
- Sereda, M, Hoare D, Nicholson R, Smith S, Hall D. (2015). Consensus on Hearing aid candidature and fitting for mild hearing loss, with and without tinnitus: Delphi Review. Ear & Hearing, July/Aug. Vol 36, issue 4, pp 417-429.






“How critical is the audiogram to a successful hearing aid fitting?” I would say it is a starting point. What is more significant is whether their devices improve hearing in situations that are important to the user. Sergei Kochkin called this MELU (Multiple Environmental Listening Utility). For this to happen users need access to a telecoil. That is, if they want to hear well in public venues (such as auditoria and houses of worship). The improvement they want and crave cannot be delivered by an ear-level mic microphone. This is a physics issue, not a sound processing or programming issue. In those public places, as well as TV rooms, users of OTC and hearing instruments would do well to make sure they have access to a telecoil. That way they can benefit from hearing loops. In a hearing loop, the audibility and clarity can be jaw-dropping. In a hearing loop, some users may hear better than their normal hearing seatmates.
What about the REM? I mean…let’s face it, anyone who fits a hearing aid without doing REMs is doing a mediocre fitting/job. So if we say that an Audiogram is not very accurate and every manufacturer’s fitting formulae is different…doesn’t it sound logical that Real-Ear Measures are a key point to accurately fit hearing aids to each individual’s acoustic parameter and needs?
OTC Hearing aids are here, yes. But so are cheap Suits from any discounter: You get what you pay for. If you don’t care nobody can tell you not to buy it. We can’t stop it from happening but it’s an opportunity for the traditional hearing care industry to provide a better service…
REM would be good, but studies have shown that only about 38% of audiologists perform this at all, and I could be wrong, but I believe I read that only about 50% or so of audiologists even have REM equipment. The article by Azah H. and Moore BCJ. (2007). The value of routine real ear measurement of the gain of digital hearing aids. Journal of the American Academy of Audiology, 18(8), 653-664 is something that all audiologists should read.
Re telecoils, I also believe that they should not ignored. I received some PSAPs the other day that have very nice auto telecoils in them.
Wayne, great to hear that some PSAPs have included a telecoil. But, someone needs to tell the MFRs of those devices that auto-coils do work in hearing loops. What make? I will be happy to do so. To hear in a loop, consumers need access to a manual telecoil. Re: REM – consumers need to be educated about this and encouraged to demand it. The same with speech-in-noise testing. I usually refer consumers to a comprehensive article by Cynthia Compton-Conley, where best practices are spelled out: http://www.hearingloss.org/sites/default/files/docs/HLM_JulAug2015_Compton-Conley(dot)pdf
Audiologists may want to list their comprehensive fitting, verification and validation services on HearingTracker.com
Wayne, great to hear that some PSAPs have included a telecoil. But, someone needs to tell the MFRs of those devices that auto-coils do work in hearing loops. What make? I will be happy to do so. To hear in a loop, consumers need access to a manual telecoil. Re: REM – consumers need to be educated about this and encouraged to demand it. The same with speech-in-noise testing. I usually refer consumers to a comprehensive article Cynthia Compton-Conley wrote for the JulAug 2015 issue of Hearing Loss Magazine, where best practices are spelled out.