Learning the effects of chemotherapy medications and the proper procedure for monitoring ototoxicity during cancer treatment can be a good way for an audiology practice to differentiate itself from other practices in the area. Due to our practice’s new relationship with a local cancer treatment center, we  have encountered numerous cases of ototoxicity from cancer treatment in our clinic. McKeage (1995) states that 70% to 100% of chemotherapy patients using the “platinum”
have encountered numerous cases of ototoxicity from cancer treatment in our clinic. McKeage (1995) states that 70% to 100% of chemotherapy patients using the “platinum”  drugs will suffer high-frequency hearing losses and tinnitus as a result. Audiological monitoring of chemotherapy patients during treatment is considered routine clinical practice to determine when the physician needs to cease or adjust the treatment. Other chemotherapy medications and procedures that require careful audiological monitoring include use of aminoglycocides, diuretics from the “loop” classification, radiation to the head, especially when the beam is directed toward the brainstem or the ear, and surgery involving the brain, ear, or auditory nerve. .
drugs will suffer high-frequency hearing losses and tinnitus as a result. Audiological monitoring of chemotherapy patients during treatment is considered routine clinical practice to determine when the physician needs to cease or adjust the treatment. Other chemotherapy medications and procedures that require careful audiological monitoring include use of aminoglycocides, diuretics from the “loop” classification, radiation to the head, especially when the beam is directed toward the brainstem or the ear, and surgery involving the brain, ear, or auditory nerve. .
Chemotherapy
There are many different types of chemotherapy drugs used in a variety of ways to treat different types of cancer. Chemotherapy benefits include  destroying cancer cells, shrinking existing tumors, and preventing cancer cells from thriving and multiplying. The goal of these procedures is to prevent or slow down the progression of the disease to assist in the extension of life. The medications used in these treatments can have serious side effects and, thus, physicians must weigh the benefits of chemotherapy against the risk factors and expected outcomes.
destroying cancer cells, shrinking existing tumors, and preventing cancer cells from thriving and multiplying. The goal of these procedures is to prevent or slow down the progression of the disease to assist in the extension of life. The medications used in these treatments can have serious side effects and, thus, physicians must weigh the benefits of chemotherapy against the risk factors and expected outcomes.
A cancerous tumor is a collection of abnormally growing cells. When physicians use chemotherapy to shrink an  existing tumor, the expected benefit is to improve the patient’s quality of life by decreasing the pain and pressure caused by the tumor. Although the tumor is likely to continue to grow or return, shrinking a tumor can control the disease to the extent that a cancer patient will live longer, more pain-free life.
existing tumor, the expected benefit is to improve the patient’s quality of life by decreasing the pain and pressure caused by the tumor. Although the tumor is likely to continue to grow or return, shrinking a tumor can control the disease to the extent that a cancer patient will live longer, more pain-free life.
Chemotherapy may also be used to shrink tumors prior to surgery or radiation treatments. Since cancer cells can grow and spread quickly, chemotherapy can help prevent cancer cells from spreading from the original site to other parts of the body. At times, chemotherapy is used to destroy any cancerous cells that remain in the body after radiation treatment or surgery, and may also be used to assist in the effectiveness of radiation treatments. Chemotherapy is often the treatment used when cancer that was eliminated returns to the same area or to another part of the body. In advanced stages of cancer, chemotherapy may be used simply to relieve symptoms and improve quality of life even though it cannot extend life.
Chemotherapy began in the late 1940s when Dr. Sidney Farber (1903-1973), a pediatric pathologist at Harvard Medical School, was working on a research project funded by a grant from the American Cancer Society. Dr. Farber carried out both the preclinical and clinical evaluation of aminopterin, a folate antagonist in childhood acute lymphoblastic leukemia. In 1948, Farber was the first to demonstrate that the induction of clinical and hematological remission in this disease was achievable. These findings promoted Farber as the “father” of the modern era of chemotherapy for neoplastic disease, having already been recognized for a decade as the “father” of modern pediatric pathology.
These observations led to the development and use of other chemotherapeutic agents, either singly or, more effectively, in combination for treating childhood and adult malignancies. Throughout the 1950s and ’60s, Farber continued to make advances in cancer research, notably the 1955 discovery that the antibiotic actinomycin D and radiation therapy could produce remission in Wilms’ tumor, a pediatric cancer of the kidneys. And it was during this period that he took his persuasive powers to a national stage. Beginning in the early 1950s, and continuing until his death in 1973, Farber became a star presenter at Congressional hearings on appropriations for cancer research. A compelling speaker, he was very successful in his efforts and a champion for those with cancer.
Audiology Implications
Sometimes there is no choice in the matter. Even though there are known ototoxic side effects, oncologists will review the case and decide that chemotherapy is essential to sustain the patient’s life, relieve symptoms, or improve their quality of life, even knowing that there will likely be damage to the cochlea and/or other areas of the hearing system. In such cases, audiologists are usually asked to monitor the  patient’s hearing. Typically the oncologist will request a pre-evaluation prior to the administration of the chemotherapy to establish a hearing baseline and then hearing is
patient’s hearing. Typically the oncologist will request a pre-evaluation prior to the administration of the chemotherapy to establish a hearing baseline and then hearing is  monitored during the administration, and for some time afterwards to record the changes.
monitored during the administration, and for some time afterwards to record the changes.
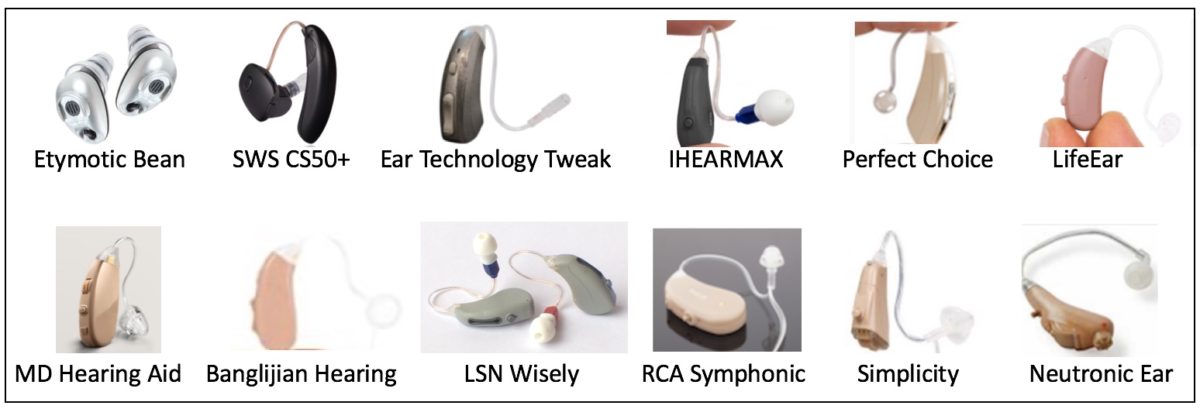
Prior to beginning an ototoxicity monitoring program, it’s a good idea to meet with the referral sources and discuss the program and how the referrals will be conducted, as some medications vary in the time limitations necessary to affect the hearing baseline testing. The specific procedures should be discussed and considered, as most hearing routine hearing evaluations are conducted between 250 and 8000 Hz., and do not offer early warning as to the effect. To see these early effects the literature suggests that high-frequency audiometry from 9000-20,000 Hz can detect hearing reductions earlier, allowing the physician to make critical decisions as to ceasing or modifying the chemotherapy before it reaches the critical frequencies for speech. Additionally, otoacoustic emissions testing is also beneficial in detecting early outer hair cell damage that occurs with hearing loss due to ototoxicity. Monitoring hearing during chemotherapy and other cancer procedures allows the patient and the audiologist to  plan an aural rehabilitation program for after-treatment. At the end, of the treatment, it may be necessary to re-evaluate the patients hearing at intervals to determine of the impairment progresses.
plan an aural rehabilitation program for after-treatment. At the end, of the treatment, it may be necessary to re-evaluate the patients hearing at intervals to determine of the impairment progresses.
Prior to beginning a monitoring program for chemotherapy patients audiologists need to take time to study the monitoring process, review the literature regarding ototoxicity and the effects of various medications on the audiovestibular system and the effects of various amplification circuits relative to the specific requirements of a damaged cochlea.
References:
Chemocare.com (2015). Cisplatin. Scott Hamiliton Cares Initiative. Retrieved March18, 2015: http://chemocare.com/chemotherapy/drug-info/cisplatin.aspx#.VQb7SY7F8bM
Curesearch for Children’s Cancer (2015). Hearing Problems. Retrieved March 18, 2015: http://curesearch.org/Hearing-Problems
McAdams, M. (2013). Chemotherapy benefits. Livestrong.com Retrieved March 18, 2015: http://www.livestrong.com/article/125084-chemotherapy-benefits/
McKeage, M. (1995). Comparative adverse effect profiles of platinum drugs. Drug Safety. Volume 13, number 4, pp 228-244. Retrieved March 15, 2015: http://link.springer.com/article/10.2165/00002018-199513040-00003#page-1
Images:
Moment of Science (2003). Cancer cells and chemotherapy. Retrieved March 18, 2015: http://indianapublicmedia.org/amomentofscience/cancer-cells-and-chemotherapy/
Weiss, T. (2013). Sensorineural hearing loss and ototoxic medications. Disabled World. Retrieved March 18, 2015: http://www.disabled-world.com/disability/types/hearing/snhl.php