Canalith Repositioning (CRP), more commonly referred to as the Epley maneuver, has become the “go to” treatment for the complaint of positional vertigo. I have been at this long enough to see the transition from skepticism that any condition could be quickly treated by lying down and rolling over in bed, to the current habit of people being treated for BPPV even though they have not undergone any related diagnostic testing. That sounds worse than it really is because the vast majority of patients that complain of something sounding vaguely like BPPV do, in fact, have BPPV in the posterior canal. Additionally, there is very little chance, and no reports, of harm associated with doing the Epley maneuver at home or in the practitioner’s office.
We have seen a handful of patients with worrisome brain and/or brainstem pathology that were never examined for positional nystagmus and sent home with instructions to repeatedly provoked their symptoms, but this a less than 1% issue.
The most likely, and very common downside to such widely available treatment instructions is that many patients are sent home with dated instructions (Brandt-Daroff exercises are not nearly as effective as a home Epley), or got the correct exercises but are doing them incorrectly.
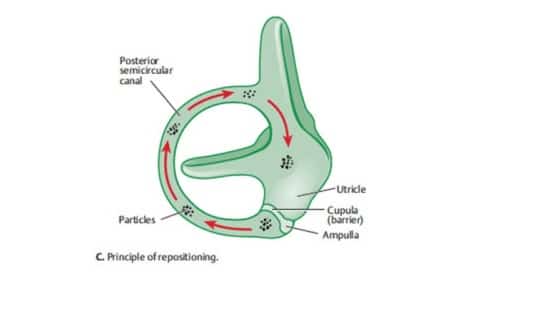
Brandt-Daroff exercises are still in use, I suspect, because they were the first therapy treatment offered for BPPV. As early as 1980, the exercises were offered in hopes of “habituating” the symptoms triggered by position change, meaning that Drs. Brandt and Daroff theorized that over time, people would adapt or “get used to” their symptoms. Soon enough, they noted that some patients improved too rapidly to be explained by habituation, and suspected a “dispersion of otolithic debris.” So, where does the otolithic debris go?
There are a few theories to consider, but one seems more plausible than the others. Zucca proposed the theory, and provided some impressive evidence, that otoconia dissolve in endolymph (view that article here). This is supported by the natural history of BPPV, as well as the rapid improvements seen after CRP. Otoconia in the semi-circular canal are bathed in endolymph, but at a much lesser fluid volume than in the vestibule.
BPPV Vertigo Treatment: What Happens to the Otoconia?
As I describe to patients, the debris can survive for weeks in the canal, but typically dissolves within less than 24 hours in the vestibule. I use the analogy of a cup of coffee and a teaspoon of sugar. I point out that if you put a drop or two of coffee in a teaspoon of sugar each day, it would take weeks for the sugar to dissolve. If you put the teaspoon of sugar in the cup of coffee, it dissolves in a matter of seconds. The only difference being the fluid volume, and there is much greater fluid volume of endolymph in the vestibule.
We know that BPPV eventually resolves whether the otoconia stay in the canal or are moved to the vestibule. It just resolves a lot faster after the otoconia has been moved to the vestibule.
There are two other theories that are less clear, or seem less likely than the theory proposed by Zucca. One theory is that the otoconia “stick” to the utricle when entering the vestibule. I have seen too many canal conversions, from posterior to horizontal canal, and recently one from horizontal to anterior canal) to believe that the otoconia stick to the utricle very easily. BPPV occurs because otoconia come loose from the utricle.
Another theory is that “dark cells” absorb the otoconia. There is no recent literature addressing this theory, so I will pass on exploring this any further for now.






Have you ever considered that like a snow globe and like any dense materials the otoconia may fall to the base of the utricle and work their way into the endolymphatic duct and then into the endolymphatic sac? Looking at the models of inner ears, there is a logical pathway that the debris falls to the base of the otolith. To assume that crystals just are absorbed into the endolymph suggests that the existing otoconia on the utricle and saccule would just dissolve within the endolymphatic fluid in their respective anatomical regions. Matter can neither be created nor destroyed someone once said…
Hi Brian:
Of course, it would be presumptuous to not consider alternatives that you mention. However, there is evidence that otoconia dissolve in endolymph as described in the Zucca article. Whether that occurs in the vestibule or endolymphatic sac is unknown.