Vestibular schwannoma, also known as acoustic neuroma, refers to a benign tumor that arises from the Schwann cells or nerve sheath on the vestibulocochlear nerve. For consistency and brevity, I will refer to these tumors as VS for the remainder of this blog. Other masses can occur within the internal auditory canal, however, VS are the most prevalent and for simplicity we will be discussing VS only.
These masses are typically slow growing and most often only impact one ear. Typical symptoms include progressive unilateral hearing loss, tinnitus, pressure or fullness in the ear, and dizziness/imbalance. If a mass like this is not treated it can grow large enough to impact brainstem function, which can be potentially life threatening. Diagnosis is typically made by MRI of the brain, but additional measures of hearing and vestibular function are often utilized to aid in the diagnosis. Treatment typically includes gamma knife radiosurgery for smaller VS, while surgery is typically recommended for larger tumors.
Early identification and treatment of these tumors is typically preferrable due to the less invasive nature of gamma knife vs. traditional surgery.
Epidemiology of Vestibular Schwannoma
The incidence of VS is estimated to be around 0.6 per 100,000 to 1.09 per 100,000, but there is some evidence that the incidence is rising. The rise in the incidence is likely at least partially related to better imaging techniques and more widespread use of imaging. The incidence increases with age and the average age of diagnosis is around 60 years old.
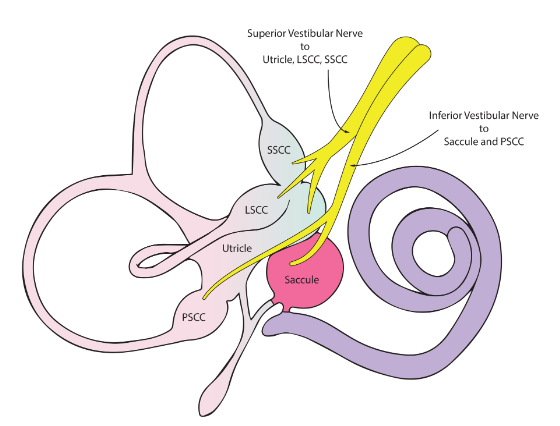
Image credit: ENT Education Swansea
There is no significant difference in incidence based on gender. There is at least some evidence to support that African Americans have a lower incidence of VS while Asian Pacific Islanders have a higher incidence.
It is generally agreed upon that most of these masses arise on the vestibular portion of the vestibulocochlear nerve. Rarely does a VS arise from the cochlear or facial nerve, hence why they are most often referred to as a vestibular schwannoma. There is mixed evidence to support whether the superior branch or inferior branch of the vestibular nerve is more likely to be impacted.
Some studies show a clear preponderance for the inferior branch being impacted while others show a more even split (nearly 50/50) between which branch(s) are the primarily impacted portion of the nerve. An image can be found below for those unfamiliar with inner ear anatomy.
Diagnostic Assessment
There are medical contraindications, monetary limitations and lack of access that prevent some individuals from undergoing MRI, which forces the clinician to rely heavily on other measures. We encounter this frequently at a clinical level, which begs the question, just how sensitive are these test measures at detecting a VS? A hearing evaluation is likely to be completed as a first line measure and most individuals with a VS will have some degree of sensorineural hearing loss in the impacted ear.
 It is also common for those with VS to report tinnitus in the impacted ear. One of the more frequently utilized measures to assess vestibulocochlear nerve health is the auditory brainstem response (ABR). The ABR is an evoked potential that measures how the auditory pathways are relaying information to the brain. This test requires the patient to wear surface electrodes on the skin while a stimulus/sound is presented to the ear. These electrodes measure how the auditory pathways are sending the sound to the brain. ABR is frequently utilized in hearing assessment for infants or for patients otherwise unable to undergo a standard hearing evaluation in a sound booth.
It is also common for those with VS to report tinnitus in the impacted ear. One of the more frequently utilized measures to assess vestibulocochlear nerve health is the auditory brainstem response (ABR). The ABR is an evoked potential that measures how the auditory pathways are relaying information to the brain. This test requires the patient to wear surface electrodes on the skin while a stimulus/sound is presented to the ear. These electrodes measure how the auditory pathways are sending the sound to the brain. ABR is frequently utilized in hearing assessment for infants or for patients otherwise unable to undergo a standard hearing evaluation in a sound booth.
Prior to the advent of MRI the ABR was the primary measure used to assess for VS. The ABR can still be useful in cases where an MRI is unable to be obtained or the risk for a nerve mass seems less likely.
ABR Assessment for Vestibular Schwannoma
I reviewed five studies which investigated the sensitivity of the ABR in detecting a VS and averaged the results. The average overall sensitivity of ABR in detecting VS was 87%. In cases of larger VS (>10 mm) the average sensitivity was 95% and in cases of smaller VS (<10mm) the average sensitivity was 69%. This literature review suggests that ABR is better at detecting larger VS (>10mm) and not as sensitive in detecting smaller VS (<10 mm).
While MRI will remain the gold standard for identifying VS, it is important to note that ABR can be a useful measure in cases where MRI is unable to be performed.
Links to these studies can be found below.
- Acoustic Neuroma (Vestibular Schwannoma): An Overview of Symptoms, Diagnosis, and Treatment
- Evaluating ABR Sensitivity in Diagnosing Vestibular Schwannoma: Key Findings
- Auditory Brainstem Response and Acoustic Neuroma Detection: Diagnostic Insights
- Using ABR as a Screening Method for Vestibular Schwannoma: Effectiveness and Limitations
- How Sensitive is ABR for Detecting Vestibular Schwannoma? A Review of Recent Data
Vestibular Function Tests
Measures of vestibular (inner ear balance) function are also often completed for patients suspected to have a VS. Most individuals with a VS will have abnormal measures of vestibular function, particularly with a larger VS. It has been shown 86% of individuals with VS will have abnormal vestibular function test measures, even with more basic vestibular testing. In recent years more comprehensive testing of the vestibular system has become available, further increasing the sensitivity of vestibular testing.
The most widely utilized vestibular function test is the caloric irrigation. This test involves stimulating the inner ear organs with temperature change, using warm and/or cool water or air. This creates a thermal affect and results in eye movement or nystagmus that can be recorded. This nystagmus can then be compared to normative data and between the ears to determine if there is asymmetry or weakness. An older study showed 82% of individuals had abnormal caloric testing while a more recent study showed that 93% of individuals had abnormal caloric measures with VS.
The video head impulse test or vHIT is also seeing more widespread use in assessing vestibular function. This test involves the patient visually fixating on a stationary object while the examiner moves the patients head rapidly.
A healthy inner ear vestibular system will allow the patient to maintain focus, while a dysfunctional inner ear leads to loss of visual focus with rapid unpredictable head movement. The vHIT allows the examiner to measure for any deficiencies in this reflex pathway.
One study showed that vHIT was 80% sensitive while another showed it was 85% sensitive in cases of VS.
Vestibular evoked myogenic potentials (VEMP) involve stimulating the inner ear structures with loud sound or vibration to the skull. The inner ear sends information all over the body for stable vision during movement (VOR) and to the lower extremities for postural control (VSR). We can measure alterations in muscle activity when stimulating the ear through testing known as a VEMP. One study showed VEMP to be 73% sensitive while another showed sensitivity ranging from 65% to 75%, dependent on which VEMP measure was utilized.
A more comprehensive vestibular battery has been shown to increase the sensitivity of testing at detecting VS to 97%. Comprehensive vestibular testing utilized in conjunction with ABR likely further increases the sensitivity. This review doesn’t encompass all measures of vestibular and auditory function that could potentially be utilized, but it does provide a summary of some of the more commonly utilized measures and their utility in the assessment for individuals with VS. Vestibular function tests and ABR still clearly have a place in the assessment of patients with suspected VS.

Brady Workman, AuD, is an audiologist in the Balance Disorders program at Wake Forest Baptist Health Center. He has authored several articles relating to balance and vestibular disorders as a regular contributor and co-editor of the Dizziness Depot at Hearing Health & Technology Matters. Brady received his doctorate of audiology from East Tennessee State University in 2018 and is licensed by the North Carolina Board of Examiners for Speech Language Pathologists and Audiologists and is a fellow of the American Academy of Audiology.






