Many of us have experienced several seconds where we hear a ringing sound, but there is no evident source of the sound. For most of us, this sound goes away after several seconds, but for some the sound is much more persistent and bothersome. The sound perceived is what is known as tinnitus.
Tinnitus refers to the perception of a sound without any external source of the sound.19 Tinnitus is common, with recent estimates showing 10 to 15% of adults in the United States report experiencing tinnitus.7,10 It seems likely that these estimates are low and comprise those with more persistent or bothersome tinnitus.
Tinnitus has a longstanding history with reports dating back to Egyptian and Babylonian civilizations. In those times it was believed that the tinnitus was due to vengeful spirits or other supernatural phenomena.4 Despite the prevalence and lengthy recorded history, there are no current treatments that silence the tinnitus, and the exact cause, or likely causes, are not fully understood.
Objective vs. Subjective Tinnitus
In general, there are two main types of tinnitus, objective tinnitus and subjective tinnitus.
Objective tinnitus is generated mechanically within the body and both the individual from whom the tinnitus is produced and other listeners can hear objective tinnitus. Objective tinnitus can be caused by vascular anomalies or involuntary contractions of middle ear muscles, but is much less common than subjective tinnitus.8 Sometimes one may perceive their objective tinnitus as a pulsing sound that seemingly fluctuates with their heartbeat. Pulsatile tinnitus is relatively rare but should be fully investigated to determine if it is due to a potentially worrisome cause.18
Subjective tinnitus will be our primary focus as it is much more common.8 Subjective tinnitus can only be heard by the individual with the tinnitus and is most often believed to be associated with damage to the auditory (hearing) system. From here forward, all mentions of tinnitus will be in reference to subjective tinnitus, but will be referred to only as tinnitus for simplicity.
For many, tinnitus sounds like a high pitch ringing noise, but can also sound like crickets, buzzing, hissing, humming, clicking, or roaring. Tinnitus may sound as if it coming from one ear, both ears, or for some, it may be unclear where the sound is located. Some individuals only perceive their tinnitus in quiet scenarios, while others may notice it at all times, which can have a negative impact on their ability to sleep or concentrate. Tinnitus is different from an auditory hallucination in that the tinnitus sound is an otherwise meaningless sound.
What Causes Tinnitus?

Roughly 15 percent of all adults in the United States have tinnitus.
Tinnitus is a symptom rather than the primary disease process. Most individuals are not born with tinnitus, suggesting a change along the auditory pathway to cause the tinnitus. It has been estimated that as many as 90% of those with tinnitus have some degree of hearing loss, and this is most prevalent in those with greater hearing loss.5,6
Tinnitus does not always occur with hearing loss and can also be caused or made worse by by head or neck injury, stress, anxiety, other ear disorders, medications or many other vascular and/or neurological conditions. Recent evidence also shows changes in the central (brain) auditory pathways with tinnitus, likely making the generation and preservation of tinnitus much more complex than originally thought.8
Ear Anatomy Basics
The hearing portion of the ear has three main components including the outer, middle and inner ear. The outer ear is the portion of the ear that can be readily seen when looking at someone and consists of the pinna and ear canal, both of which are responsible for capturing and funneling sound energy to the eardrum.
The middle ear consists of three bones called ossicles attached on one end to the eardrum and on the other to the inner ear. When the sound energy hits the eardrum, it vibrates and moves the ossicles. The middle ear bones work like a lever, pushing in on the fluid filled inner ear.
The inner ear organ of hearing is called the cochlea, which consists of several fluid-filled tunnels with small hair cells within one of the tunnels. As a result of the middle ear bones pushing into fluid filled inner ear, this creates a wave of fluid movement, which stimulates these hair cells.
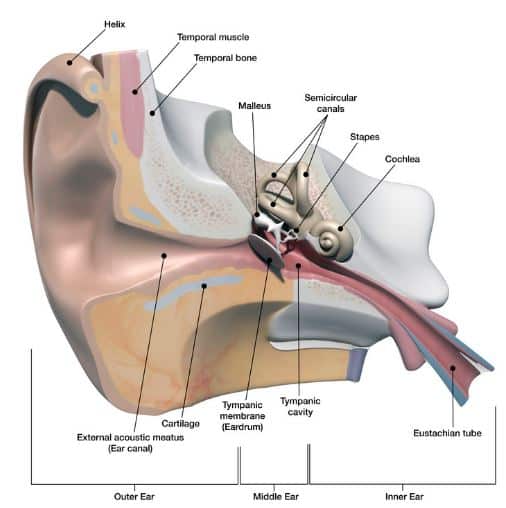
The hair cells work to capture and extract the incoming sound energy to then be sent to the brain for perception. The hair cells within the cochlea are organized by pitch, with the high-pitch hair cells being closest to the middle ear and the low-pitch hair cells being farthest from the middle ear.
In other words, different hair cells in the cochlea are responsible for extracting different pitches from the fluid wave. Most often, when one has hearing loss related to noise and/or aging, it is what is called a sensorineural hearing loss and is because of damage to the hair cells. Sensorineural hearing loss is the most common type of hearing loss and when related to noise exposure or aging, it typically affects the higher pitch hair cells first.
Many individuals experience a tinnitus sound that is close in pitch to the damaged area within the cochlea.
Assessment of Tinnitus
Because most individuals with tinnitus have at least some degree of hearing loss, a hearing test should be completed to determine if hearing loss is present. Prior to completing a hearing test, one should ensure there are no obvious causes for decreased hearing or tinnitus, such as an over accumulation of earwax in the ear canal. If an earwax obstruction is noted, this should be removed prior to further evaluation.

Key to any tinnitus assessment is a comprehensive audiology exam
A comprehensive hearing evaluation consists of establishing frequency (pitch) specific hearing thresholds for sounds presented down the ear canal with either headphones or inserts (air conduction) and via vibrations presented to the skull (bone conduction) to determine the type of hearing loss, as well as word recognition testing. A hearing test is usually completed by an audiologist, a masters or doctoral level professional that specializes in the diagnostics and non-medical management of ear disorders, but may also be completed by a technician in some settings.
Most often, you do not need to see a physician for tinnitus unless you have a difference in hearing between ears, a potentially medically correctable hearing loss, sudden hearing loss, facial weakness or paralysis, dizziness symptoms, drainage from the ear, and/or a sensation of pressure or pain in their ears.
If any of the above “Red Flags” are noted, additional assessment by an otolaryngologist, a physician with specialty in disorders of the ears, nose and throat, would be warranted.
Individuals with a similar amount of sensorineural (inner ear) hearing loss between the ears, most often related to noise exposure or aging, do not typically need physician evaluation. For these individuals, additional assessment can include subjective questionnaires to better understand and monitor any changes in the subjective impact the tinnitus has on one’s life.
Additional assessment to better understand the pitch and loudness of the tinnitus can also be completed to best assist with management of the tinnitus. An audiologist most often completes this additional assessment.
“Normal Hearing” and Tinnitus
There is a growing body of literature showing individuals that have tinnitus with a “normal” hearing evaluation, without any other obvious cause for the tinnitus. There have been recent theories for why this might occur, with one of them being called synaptopathy or “hidden hearing loss”.12,15
This theory proposes that the neural synapse, or communication point between the hair cell and the auditory nerve, can become damaged. This damage at the level of the synapse is enough to cause the individual to perceive tinnitus and likely have some degree of hearing difficulty, but not enough to cause the audiogram to be abnormal.12,15
At the time of writing this there is no gold standard for the assessment for “hidden hearing loss”.
Management of Tinnitus
 There is no magic treatment to silence tinnitus. This is due to tinnitus most often being related to sensorineural hearing loss, which at present, can only be managed with hearing aids or cochlear implantation dependent on the amount of hearing loss. The hair cells damaged within the inner ear in sensorineural hearing loss cannot be regenerated currently in humans.
There is no magic treatment to silence tinnitus. This is due to tinnitus most often being related to sensorineural hearing loss, which at present, can only be managed with hearing aids or cochlear implantation dependent on the amount of hearing loss. The hair cells damaged within the inner ear in sensorineural hearing loss cannot be regenerated currently in humans.
Neither hearing aids nor cochlear implantation truly treats the damaged inner ear; these devices simply provide greater access to sounds through amplification. Also, the generation of tinnitus appears to be complex and multi-faceted, involving changes in the central auditory pathway neural firing patterns, making it unlikely that this would immediately silence one’s tinnitus, even if the hair cells could be regenerated.8
That is not to say that nothing can be done to help manage tinnitus. It has long been a recommendation to “mask” or cover one’s tinnitus sound with another, less bothersome noise. The use of background noise to mask bothersome tinnitus dates back to French physician Jean Marc Gaspard Itard, who recommended his patients utilize a roaring fire to mask out their tinnitus in the 1800’s. The use of a tinnitus masker is still recommended by most practitioners today for those with bothersome tinnitus. Most individuals nowadays utilize either smart phone applications or stand alone masking devices to achieve these masking effects.
Most practitioners agree that hearing aids are useful in managing tinnitus, especially for those who also have sensorineural hearing loss.16 By amplifying soft sounds as in the case of hearing aids, the hearing aids works as a tinnitus masker of sorts. There are also hearing aid programming protocols to maximize the benefit of hearing aids for tinnitus management.17 Many modern hearing aids have a tinnitus masker option, allowing for further masking with the hearing aids.
One’s own subjective evaluation of their tinnitus can have a large impact on how bothersome it is to them.10 That is to say that ones self-evaluation of the tinnitus can evoke strong emotional responses from within the brain. If one evaluates their tinnitus as a vengeful spirit, which is sure to mean their impending demise as was common in Babylonian times, then their tinnitus may be evaluated as a sound of extreme importance, associated with negativity and fear. Thus, one’s evaluation of the tinnitus sound can evoke extreme conditioned emotional responses dependent solely upon how it is assessed, which has a direct relationship to how bothersome it is to the individual. This bi-directionality of tinnitus is of extreme importance in the management of tinnitus and it is imperative that there be at least some degree of counseling that aims to promote a correct evaluation of ones tinnitus. Strategies that may be usefully implemented in tinnitus management along with hearing aids and masking options include cognitive behavioral therapy9 and mindfulness training.14
“Tinnitus, often linked to sensorineural hearing loss, lacks a definitive cure, as damaged inner ear hair cells cannot be regenerated in humans. However, management strategies such as masking with background noise and using hearing aids show promise in reducing its impact.”
There is currently a recommendation against the use of dietary supplements and/or the use of antidepressant medications for routine management of tinnitus. Other treatments, like transcranial magnetic stimulation are also not recommended. There is currently not a professional consensus on the use of acupuncture for tinnitus management.19
{interested readers can check out a discussion on dietary supplements for tinnitus by Dr. Robert DiSogra in the video below}
Who is at Risk for Tinnitus?
Anyone that is exposed to excessive levels of noise, whether recreationally or occupationally is at an increased risk for developing tinnitus. Those with health conditions like high blood pressure and diabetes are at increased risk for hearing loss, increasing the likelihood of developing tinnitus.1,2
Those with frequent earwax build up can notice tinnitus if their ear canal becomes full of wax. Also, anyone with progressive hearing loss, temporomandibular joint disorder (TMJ),13 other ear conditions, as well as those taking ototoxic (ear toxic) medications is at increased risk for developing tinnitus.3

How to Prevent Tinnitus?
Protecting one’s hearing is the best way to reduce the likelihood of having tinnitus. In an occupational setting, most businesses in the United States require hearing protection if the noise levels associated with the job have been determined as unsafe. Anyone with questions regarding exposure to potentially dangerous levels of noise can consult the Occupational Safety and Health Administration (OSHA) or US National Institute for Occupational Safety and Health (NIOSH).
Also, one can always consult a local audiologist to further discuss when hearing protection is necessary, as well as what hearing protection devices would be appropriate depending on the scenario. When in situations of excessive noise, it is always best to play it safe and wear hearing protection.
One has little influence on tinnitus related to age or genetic hearing decline, but monitoring of the hearing should be completed. Those with high blood pressure and/or diabetes should work with their doctor in controlling these conditions to lessen their impact on their hearing and reduce their chances of developing tinnitus. Those with tinnitus related to medications should consult with their primary care provider and otolaryngologist to determine necessity and dosages of the medications. Stress and anxiety do have the potential to make ones tinnitus more noticeable or bothersome and should also be treated to reduce the impact on ones tinnitus.
When to Seek Help
Anyone experiencing frequent or bothersome tinnitus should seek professional assessment to determine the cause of the tinnitus.
Tinnitus is most often a symptom of hearing loss related to aging or noise exposure, but it can also occur with many more disorders, making assessment necessary to determine the cause.
References
- Agarwal, Y., Mishra, A., Jagade, M., Kasbekar, V., & Nagle, S. (2013) Effects of hypertension on hearing. Indian J. Otolaryngol. Head & Neck Surg.. 65(3) 614-618.
- Bainbridge, K.E., Hoffman, H.J. & Cowie, C.C. (2008) Diabetes and hearing impairment in the United States: Audiometric evidence from the national health and nutrition examination survey, 1999 to 2004. Annals of Internal Medicine. 149(1): 1-10.
- Bisht, M. & Bist, S.S. (2011) Ototoxicity: The hidden menace. Indian J. Otolaryngol. Head Neck Surg.. 63(3): 255-259.
- Feldmann, H. (1988). Pathophysiology of tinnitus. In: Kitahara M, ed. Tinnitus: Pathophysiologyand Management. Tokyo: Igaku-Shion, 7-35.
- Fowler, E.P. (1944) Head noises in normal and disordered ears: significance, measurement, differentiation and treatment. Archives of Otolaryngology. (39): 490–503.
- Han, B.I., Lee, H.W., Kim, T.Y., Lim, J.S., Shin, K.S. (2009) Tinnitus: characteristics, causes, mechanisms, and treatments. Journal of Clinical Neurology, (5) 11–9.
- Henry JA, Dennis KC, Schechter MA. (2005) General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. 48:1204-1235.
- Henry, J.A., Roberts, L.E., Caspary, D.M., Theodoroff, S.M. & Salvi, R.J. (2014) Underlying mechanisms of tinnitus: Review and clinical implications. Journal of the American Academy of Audiology. 25(1): 5-126.
- Hesser, H., Weise, C., Westin, V.Z., & Andersson, G. (2010). A systematic review and meta-analysis of randomized controlled trials of cognitive–behavioral therapy for tinnitus distress. Clinical Psychology Review, 31(2011): 545-553.
- Hoffman HJ, Reed GW. (2004) Epidemiology of tinnitus. In: Snow JB, ed. Tinnitus: Theory and Management. Lewiston, NY: BC Decker: 16-41.
- Jastreboff, P.J. (1995) Tinnitus as a phantom perception: theories and clinical implications. In Vernon J., Moller A.R., eds Mechanisms of Tinnitus. Boston: Allyn & Bacon, 73-94.
- Kujawa, S.G. (2014). Putting the neural back in sensorineural: primary cochlear neurodegeneration in noise and aging. The Hearing Journal, 67(11)
- Mottaghi, A., Menendez-Diaz, I., Cobo, J.L., Gonzalez-Serrano, J., & Cobo, T. (2019) Is there a higher prevalence of tinnitus in patients with temporomandibular disorders? A systematic review and meta-analysis. Journal of Oral Rehabilitation. 46(1): 76-86.
- Pilipott, P., Nef, F., Clauw, L., Romree, M.D., & Segal, Z. (2012). A randomized controlled trial
- of mindfulness‐based cognitive therapy for treating tinnitus. Clinical Psychology & Psychotherapy, 19: 411-419.
- Plack, C.J., Barker, D., & Prendergast, G. (2014). Perceptual consequences of “hidden” hearing loss. Trends in Hearing. 18, 1-11.
- Shekhawat, G.S., Searchfield, G.D., & Stinear, C.M. (2013) Role of hearing aids in tinnitus intervention: a scoping review. Journal of the American Academy of Audiology, (24): 747-762.
- Shekhawat, G.S., Searchfield, G.D., Kobayashi, K., & Stinear, C.M. (2013) Prescription of hearing aid output for tinnitus relief. International Journal of Audiology, 1-9. Doi: 10.3109/14992027.2013.799787
- Sismanis A. (2011) Pulsatile tinnitus: Contemporary assessment and management. Otolaryngology & Head and Neck Surgery. 19(5): 348–357.
- Tunkel, D.E., Bauer, C.A., Sun, G.H., Rosenfield, R.M., Chandrasekhar ,S.S….. & Whamond, E.J. (2014) Clinical practice guideline: Tinnitus. Otolaryngol. Head & Neck Surg.. 151(2S): S1-S40.

Brady Workman, AuD, is an audiologist in the Balance Disorders program at Wake Forest Baptist Health Center. He has authored several articles relating to balance and vestibular disorders as a regular contributor and co-editor of the Dizziness Depot at Hearing Health & Technology Matters. Brady received his doctorate of audiology from East Tennessee State University in 2018 and is licensed by the North Carolina Board of Examiners for Speech Language Pathologists and Audiologists and is a fellow of the American Academy of Audiology.







