by Brian Taylor
“Signal & Noise” is a bimonthly column by Brian Taylor, AuD
Recall the term “good audiology” is loosely defined as a combination of science and art that cannot be duplicated by a computer algorithm. The first two Signal and Noise posts of 2017 were devoted to this concept of “good audiology” and why – even in this era of disruptive technology and service models – it is even more important than ever.
Speech Audiometry Resuscitated
This installment of Signal and Noise examines the limitations of the ubiquitous pure tone audiogram as a counseling tool and how the use of one quick speech audiometry procedure can provide important insights into hearing aid expectations and use. As you will recall from your introductory coursework in clinical audiology, speech audiometry – when properly conducted – is an effective way to evaluate the information carrying capacity of the cochlea and remaining auditory pathway.
The use of one additional low level speech test, described below, allows audiologists to resist the temptation to treat the audiogram, and instead treat the damaged cochlea.
Speech Performance-Intensity Functions
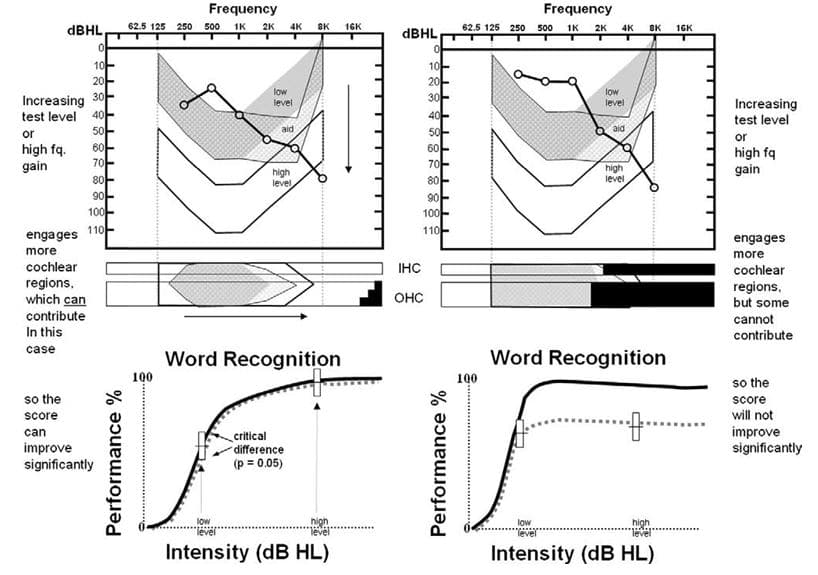
Figure 1. Audiogram, cytocochleograms and performance-intensity functions from two temporal bone cases. Described here as Patient A (left) and Patient B (right). From Halpin, C. & Rauch, S. (2009) Clinical implications of a damaged cochlea: Pure tone thresholds vs. information-carrying capacity. Otolaryngology-Head & Neck Surgery. 140, 473-476.
Conducting routine speech audiometry at two intensity levels can be a particularly effective way to explain hearing aid performance differences, especially in patients with mild to moderate, downward sloping hearing loss. This is illustrated in the Figure 1, which was reported by Halpin and Rauch in 2009 (p.474). Notice in the Figure two similar audiograms from two different patients: call them Patient A on the left and Patient B on the right.
If the clinician were to rely on standard tests – the audiogram and speech testing completed at higher intensity levels only, both patients are likely to be fitted and counseled in very similar ways. However, by conducting word recognition at a low and then high intensity level, the potential information carrying limitations of the cochlea can be established in a way that is easy to communicate to patients.
Specifically, note the results for Patient B on the right side of the Figure 1. These results, shown on the bottom right performance-intensity function, indicate the information carrying capacity for this patient is severely limited – increasing the intensity of the speech does not result in an improvement in word recognition ability.
It is this limitation that cannot be overcome with gain from hearing aids.
Using Speech Performance-Intensity Functions to Predict Hearing Aid Benefit
Most clinicians conduct speech audiometry at higher levels (see Guthrie & Mackersie, 2009 for details on best practices) as part of a routine diagnostic assessment. But as Halpin and Rauch point out, by adding a low level presentation, the clinician can demonstrate to the patient the potential for improvement from the gain provided by amplification. In their paper, they suggest conducting the procedure at two levels: 40dB HL and 70 dB HL. You could also obtain similar information by using any validated speech test, like the Quick SIN, by presenting a list at a low level and comparing it to the score you obtain at a higher intensity level.
Further, if you are wondering of it is really worth the time to make one more run of 50 words in each ear at a lower intensity level, the authors reported that of 255 cases of individuals with sloping audiograms, like the ones shown in Figure 1, a whopping 81% of cases showed no improvement at the higher intensity level.
These patients need to know that hearing aids (or any other device that restores audibility) won’t exceed their scores obtained at the higher intensity level obtained with earphones. There is a performance ceiling, uncovered by their performance-intensity function.
The bottom of Figure 1 shows the performance-intensity (PI) function for both Patient A (bottom left) and Patient B (bottom right). Note the normal PI function is in bold, while the results for both patients are represented by the dotted line. The results on the bottom left, which shows a tight match of the normal PI function, indicate the Patient A should perform quite well with hearing aids when audibility is optimized. On the other hand, as shown at the bottom right of the Figure, Patient B is likely to experience significant limitations from amplification even when audibility is optimized. Patient B will, in addition to gain, require technology that markedly improves signal to noise ratio, such as companion microphones or assistive listening devices.
Audiologists As Experts in a Time of Second Opinions
The report from Halpin & Rauch is another example of the need for “good audiology” — a clinician who can quickly and accurately conduct a validated test and use this information to make better decisions for patients. In the case of those 81% that show no improvement in performance at the higher intensity level, it is up to steadfast clinician to temper expectations, explore alternative technology that maximizes the signal-to noise ratio and not oversell the benefits of hearing aids.
As more and more patients purchase PSAPs, over-the-counter devices, and eventually, self-fitting hearing aids, it is likely clinicians will see some of these patients for a second opinion – patients that are likely to have similar performance-intensity curves like the one on the bottom right in the Figure below and are below par benefit than expected with their devices. The use of simple procedures, like presenting words at a low and a high level and plotting on the performance-intensity function, help position clinicians as experts, unbound from their hearing aid technology, willing to use data to make clear decisions for patients.
References
Guthrie LA & Mackersie CL. A comparison of presentation levels to maximize word recognition scores. J Am Acad Audiol. 2009 Jun;20(6):381-90.
Halpin C & Rauch SD. Clinical implications of a damaged cochlea: pure tone thresholds vs information-carrying capacity. Otolaryngol Head Neck Surg. 2009 Apr;140(4):473-6. doi: 10.1016/j.otohns.2008.12.021.
Brian Taylor, AuD, is audiology advisor for the Fuel Medical Group and contractor for Bose. He continues to serve as Editor of Audiology Practices, the quarterly publication of the Academy of Doctors of Audiology. During the first fifteen years of his career, he practiced clinical audiology in both medical and retail settings. Since 2005, Dr. Taylor has held a variety of leadership & management positions within the hearing aid industry in both the United States and Europe. He has published over 50 articles and book chapters on topics related to hearing aids, diagnostic audiology and business management. Brian has authored three text books: Fitting and Dispensing Hearing Aids(co-authored with Gus Mueller), Consultative Selling Skills for Audiologists, and Quality in Audiology: Design & Implementation of the Patient Experience. His latest book, Marketing in an Audiology Practice, was published in March, 2015. Brian lives in Golden Valley, MN with his wife and three sons. He can be reached at [email protected] or [email protected].
feature image courtesy of Cambridge in Color (edit)