by Barry A. Freeman, Ph.D. and Ian Windmill, Ph.D.
In the January/February AAA President’s Message, Dr. Ian Windmill discusses the recent FDA, NAS, and legislative activities surrounding affordability and accessibility to hearing care. He notes that Audiology “suffers from an access issue. There simply are not enough audiologists…to meet current demand” and we shouldn’t be surprised by these federal activities.
Anticipated Gap in Demand and Supply
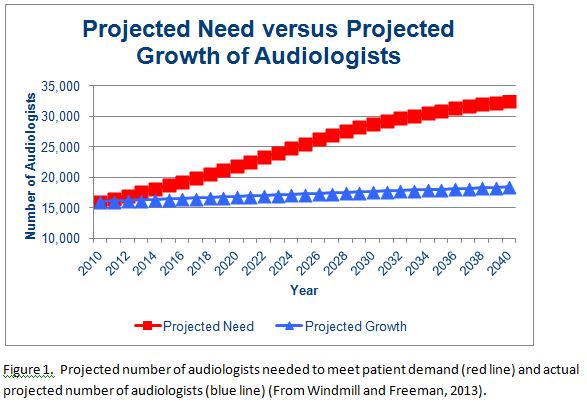
Windmill and Freeman (2013) projected a gap between patient demand and the number of audiologists available to provide the services. While they noted that the good news was that more people would seek audiology services in current and future years, the number of providers, however, would remain relatively flat or grow slowly in the coming decades.
The relatively flat projected growth presented in Figure 1 is based on anticipated graduation rates and retirements from the profession. The projected need is based on the anticipated demand for audiology services and the number of providers necessary to meet this need. The gap between the two should not be perceived as an unmet need but, rather, a challenge for the profession to improve efficiencies, increase the number of entrants to the profession, and avoid the incursion of new providers who may want to assume portions of the audiologist’s scope of practice.
 Hosford-Dunn (2017) looked at actual projections and provided some interesting insights into economic factors as to why the audiology profession may not be growing and, in fact, may be decreasing in the number of providers.
Hosford-Dunn (2017) looked at actual projections and provided some interesting insights into economic factors as to why the audiology profession may not be growing and, in fact, may be decreasing in the number of providers.
Missing Component
However, there appears to be a missing component to these projections; that is, the actual applicants to Audiology degree programs and role of the universities in preparing sufficient graduates to meet patient demand and accessibility to hearing care.
The ASHA Higher Education Services (HES) provides data on audiology education and academic programs through surveys of programs and monitoring enrollment and graduation rates (Table 1). Culling through this data provides some interesting trends and facts that may help shed additional light on the declining number of audiologists reported by Hosford-Dunn and predicted by Windmill and Freeman.
|
Year |
Applications |
Program Capacity |
Enrollment |
Total Enrollment |
Degrees Awarded |
|
2009-10 |
3,249 |
799 |
787 |
N/A |
548 |
|
2014-15 |
6,017 |
797 |
784 |
2,793 |
623 |
Table 1. Summary of Enrollment and Graduation data from 70 Au.D. programs in 2009-10 and comparing to data from 71 Au.D. programs in 2014-15.
Table 1 is a summary of data provided by HES and suggests the pool of applicants to Au.D. programs has grown by more than 85% from 2009-10 to 2014-15. This is not necessarily the total number of students applying because it is understood that many students apply to more than a single program.
Hosford-Dunn refers to the AAA’s “Ask an Audiologist” marketing campaign to enhance the profession’s brand. It appears that it has been successful as the growth in applications to Au.D. programs is significant and reveals an increasing interest in a career as an audiologist.
A Question of Capacity?
 During this same time, the capacity of Au.D. programs and enrollments have not grown and may even have declined slightly (Table 1). Program capacity and enrollments remain at an average of 11.3 students per program and, according to HES, Au.D. programs ranged in their percent of filled capacity for new enrollments to “less than 50% capacity …while others…reported exceeding 100% capacity.”
During this same time, the capacity of Au.D. programs and enrollments have not grown and may even have declined slightly (Table 1). Program capacity and enrollments remain at an average of 11.3 students per program and, according to HES, Au.D. programs ranged in their percent of filled capacity for new enrollments to “less than 50% capacity …while others…reported exceeding 100% capacity.”
While enrollments remain constant, graduation rates appear to be increasing. Of course, the 2009-10 survey was completed shortly after the final transition from master’s to doctoral degrees and some reporting programs may not have had a graduating class in 2009-10. Average graduation rates in 2014-15 were 8.7 students per program, suggesting attrition from enrollment to graduation of 20%. A review of HES surveys from the years between 2009 and 2015 reveals similar attrition rates. Only 80% of students enrolling in AuD programs are graduating and entering the profession.
A Question of Programs?
Windmill and Freeman (2013) broached the topic of audiology supply when they asked whether there are too many or too few academic programs graduating audiologists. While some may argue that there are too many academic programs in Audiology, they cautioned that the graduation rates were so low that eliminating programs might actually end up eliminating the profession since there would be an inadequate supply of audiologists to meet patient demands.
As Hosford-Dunn recently noted, “over the last eight years, the audiology labor force decreased by 3.3%.” While there is a positive trend of increased interest in the profession, program capacities and enrollments are flat. There appears to be an overall decline or, at best, flat growth in the number of practicing audiologists.
A Question of Accreditation Standards?
When academic programs were asked by HES to explain their primary reason for not increasing enrollments, they reported that the primary factor impacting enrollment was “insufficient clinical placements” and getting students the required clinical clock-hours. This is surprising and somewhat disappointing considering that all of the programs reporting data to HES are accredited by the ASHA Council on Academic Accreditation (CAA) and CAA has no reference to clinical clock hours for Audiology students in their accreditation standards and clock-hours are not required for program accreditation or student graduation.
The CAA Accreditation Standards for Au.D. programs state that programs should have “appropriate courses and clinical experiences.” The accreditation standards require,
“Doctoral-level programs in audiology must provide evidence of a curriculum that allows students to achieve the knowledge and skills…[with] the aggregate total of clinical experiences must equal at least 12 months, to include direct client/patient contact, consultation, record keeping, and administrative duties relevant to professional service delivery in audiology. The program must provide sufficient breadth and depth of opportunities for students to obtain a variety of clinical experiences in different work settings, with different populations, and with appropriate equipment and resources in order to acquire and demonstrate skills across the scope of practice in audiology, sufficient to enter independent professional practice.”
We often hear about the challenge of students attaining 1820 clinical-clock hours and that is a stated reason why academic programs will not enroll more students. However, clinical clock-hours only are required for ASHA certification and not academic program accreditation. Programs should not blame insufficient clinical experiences for clinical clock-hours as an excuse to not increase enrollments and meet the current and future needs of the profession. It is not a requirement of their accreditation standards.
How to Meet Demand
It is clear that access to hearing care will remain an issue since an increase in the number of licensed audiologists is not on the horizon with current enrollments and graduation rates. In order to avoid someone else stepping in and taking over the scope of practice, audiologists must develop and adopt technology advancements to improve clinical efficiencies and increase the role of audiology-extenders such as Audiology Assistants to meet the demand of patients.
References
Higher Education Archived Data Reports, ASHA.
Hosford-Dunn, H. 2017 New Year’s Resolution: Demand an Audiologist. HearingHealthMatters.org, Jan 3, 2017.
Hosford-Dunn, H. How Much and How Low, Audiology Workforce part 2. HearingHealthMatters.org, Jan 10, 2017.
Windmill IM & Freeman BA. Demand for audiology services: 30-yr projections and impact on academic programs. JAAA 24:407-416 (2013).
Windmill, IM and Freeman, BA. If there’s a surfeit of AuD programs, what do we do? Vote ‘em out? Hearing Health Matters, July 24, 2013.
Windmill, I.M., Where is the outrage? Audiology Today Jan/Feb, P.10-12 (2017).
Barry Freeman, PhD, is Vice President of ZPower Battery, LLC. Dr. Freeman was founding Chair of the Audiology Department and a Professor of Audiology at Nova Southeastern University and continues to maintain adjunct appointments and teach at several audiology programs. Before returning to academia in 1997, Dr. Freeman owned and practiced for twenty years at the Center for Audiology in Clarksville, TN. He is a past-president of the American Academy of Audiology and received the Distinguished Achievement Award from the American Academy in 2006. Ian Windmill, PhD, is Director of Audiology at Cincinnati Children’s Hospital Medical Center and Professor in Otolaryngology at the University of Cincinnati School of Medicine.
*featured image courtesy wikimedia commons








