Given the prevalence of hearing loss and cognitive decline in our aging population, establishing a link between these two conditions has been an area of staunch interest among researchers and clinicians for several years. In general, issues related to hearing loss has been garnering attention in the medical literate, as a December 2 editorial in the esteemed journal Lancet was devoted to the global burdens of untreated hearing loss across the age spectrum. This trend continued December 7 when JAMA Otolaryngology published a meta-analysis that examined this association between age-related hearing loss and various forms of cognitive decline, including dementia and Alzheimer’s disease.
A group of researchers from Ireland and the U.S analyzed 36 observational studies comprised of more than 20,000 adult participants from 12 countries. The objective of their work was to address the following question: Is age-related hearing loss associated with an increased risk for cognitive decline, cognitive impairment and dementia?
Unlike other similar evidence-based reviews, Loughrey and colleagues only included in their systematic meta-analysis studies that objectively measured hearing loss with pure tone audiometry.

Hearing Loss and Dementia: Connection?
In their meta-analysis, age-related hearing loss had significant associations with cognitive function in all ten cognitive domains of interest, including executive function, processing speed, semantic memory, episodic memory, and global cognition. In addition, through statistical analysis, the researchers found increased risks for Alzheimer’s disease and vascular dementia were not significant.
Although the causal mechanisms linking age-related hearing loss and cognitive decline continue to remain unclear, meta-analysis of observational studies indicate that adults with hearing loss are more at-risk for developing conditions that impact their executive functioning, memory and other cognitive abilities.
According to Loughrey and colleagues, “The pattern of decline observed in this study was consistent with estimated cognitive outcomes based on behavioral and neuroimaging research. This research reports increased recruitment of short-term memory and executive functions to aid speech perception after acquired hearing loss and concomitant decline in auditory cortex regions. This situation is estimated to lead to less decline in these functions, but greater decline in episodic and semantic long-term memory owing to reallocation of cognitive resources. Consistent with this research, we observed that hearing loss was less associated with decline in executive functions and immediate recall compared with delayed and semantic memory and was increasingly less predictive of decline in attention and immediate recall among those with greater hearing loss. In addition, semantic memory, usually maintained in older age compared with episodic memory, demonstrated a decline similar to that of episodic memory. Furthermore, the results indicated that hearing aids may benefit short-term and semantic memory.”
Reducing Risk Factors for Cognitive Decline
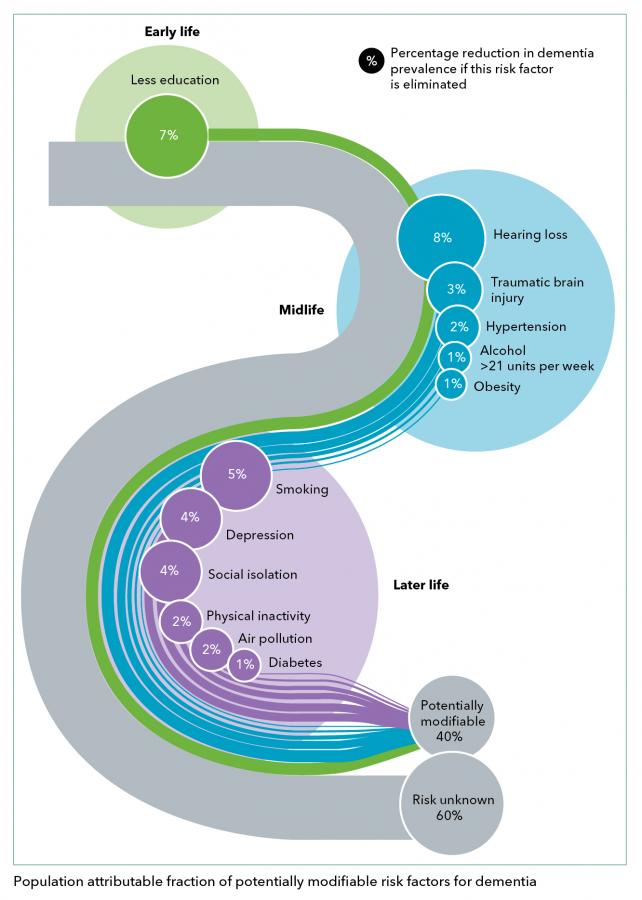
Considering the abundance of data showing a non-causal link between age-related hearing loss and cognitive decline, a public health strategy emphasizing prevention through the reduction of risk factors may be more beneficial than a healthcare strategy that relies exclusively on costly pharmacological therapy after the diagnosis of dementia.
The reduction of risk factors would include educating the public about hearing loss as a modifiable risk factor for cognitive decline, the use of hearing protection and routine hearing screenings for adults over the age of 55. Hearing care professionals, of course, play a critical role is communicating this message to the public. In turn, the public would benefit from initiatives spearheaded by hearing healthcare professionals that expand access to hearing screening programs, deliver a wider range of hearing care services and provide insurance coverage for hearing devices, especially for older adults at-risk for developing various types of cognitive decline.








Microprocessing withiin intersynaptic activity is highest at the pyramidal neurons. Hence it could be theorized that transference from perception to faster synaptic expression could be the trigger point for cognitive interpretation. Reduced blood flow has atropic
effects in the CA 1 area, and is observed during TIA episodes as damage among pyramidal neurons. It could logically follow that cognitive degeneration could begin in this area.It is still not clear if memory recall is affected simultaneously.
I think that the key to transference from regular cognition to start of changes may actually begin when the blood flow gets disrupted due to high blood pressure. All my patients with cognitive issues take blood thinners to prevent heart attack recurrences, but insults at the temporal cortex are still known to happen. Hearing loss may not be implicated as anticipated!