By Kevin M. Liebe
My fellow editor Gael Hannan, at the Better Hearing Consumer, recently published a fantastic post entitled: How to Tell Your Mother (She Has Hearing Loss).
The post begins with a conversation between a mother and a daughter, in which the daughter tries to convince her mom that it’s time for her to “do something” about her hearing loss. Here’s a brief snippet for those who missed it:
“Well, that’s what I wanted to talk…
Sorry, dear, I didn’t catch that?
…Mom, I didn’t call you, because talking on the phone is tough these days. Do you think it’s time to get your hearing checked?
Oh, not that again! Darling, I did – and she said my hearing was normal for my age. Everyone has difficulty hearing past the age of 60.
Yeah, but Mom, you’re over 70 – and that checkup was two years ago!
You know, you’re not as nice as your sister. She doesn’t stick pins in me like this.”
Does any of this ring true with you or a family member? I know it does for me.
I see these types of interactions on an almost daily basis, where you have family members, usually with the best intentions, begging their loved ones to “get a hearing aid already!” Often, however, this tactic has the opposite effect when their loved one hasn’t fully accepted that they may have hearing loss or, even more importantly, perceive the need to address what they might deem to be a “minor” problem.
As Gael puts it, “it’s not easy to control or guide another person’s hearing loss journey.” The hearing loss journey each person goes through is quite literally as unique as each individual person. That journey can, at times, mirror the various stages of the Grief Cycle (shown below):
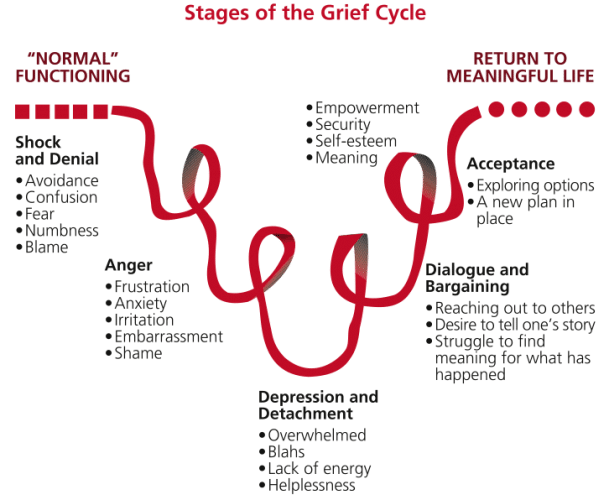
Figure adapted from the Kubler-Ross Grief Cycle (1969){{1}}[[1]]Kübler-Ross, E. (1969) On Death and Dying, Routledge, ISBN 0-415-04015-9[[1]]. Image courtesy Caregivers Connect
So how can we do a better job at convincing people to take action when they do in fact need hearing help?
Being More Effective
By coincidence, about the same time as Gael’s post published I came across a great article by Dr. John Greer Clark, Avoiding the Enemy Camp, which was posted on the online forum: Advancing Audiologic Counseling.
Is it time to re-think how we counsel? Image courtesy University of Utah
In his article, Dr. Clark suggests that to be most effective, audiologists have to approach patients from their perspective. In order to do this, it’s critically important to utilize self-assessment measures to understand how a patient is actually perceiving their hearing loss.
Despite being widely available, only a small minority of audiologists use self-assessment measures routinely.
The minimal use of these measures is likely not a malicious act on behalf of the practitioner, but more likely is explained by a perceived lack of time or not wanting to “burden” patients with additional paperwork. (Trust me, I’ve witnessed some patients go completely ballistic over having to fill out a single page of paperwork!) Yet, without this information, we may be unknowingly sabotaging the appointment before it begins and thus reducing the odds that our patient will seek further help.
For the best chance of success, Dr. Clark suggests utilizing these four steps in the consultation process:
Step 1: Review the patient’s case history and the hearing loss impact questionnaire
- Begin the initial consultation by reviewing several points on the questionnaire with the patient. This helps establish a better sense of where the patient is coming from and where they are in their individual hearing loss journey. Dr. Clark provides the following sample dialog: “I’m not sure if you have a hearing loss. As you said, others seem to mumble, and perhaps they do. Let’s do a quick hearing test to get a better picture of what’s going on.” This allows the patient to view the audiologist as a partner in the exploration of a problem and, ultimately, the discovery of a possible solution.
Step 2: Present your findings
- Contrary to what many of us were taught in school, patients often don’t want all the details as to the test findings{{2}}[[2]]Martin, F.N. (1994). Conveying diagnostic information. In J. G. Clark & F. N. Martin (Eds.), Effective counseling in audiology (pp. 38-67). Needham Heights, MA: Allyn & Bacon.[[2]]–it’s likely they won’t be able to fully absorb this information if their emotional state is high following the confirmation of a hearing loss{{3}}[[3]]Kessels, R.P.C. (2003). Patient’s memory for medical information. Journal of Royal Society of Medicine, 96,219-222.[[3]]{{4}}[[4]]Margolis, R.H. (2004) In One Ear and Out The Other. Audiology Online. https://www.audiologyonline.com/articles/in-one-ear-and-out-1102 [[4]]Prior to jumping into a discussion about hair cells, etc., consider the following dialog: “Well, I suspect you’re correct that others have bad speaking habits. But it does appear you have some hearing loss as well. Do you want the details of what I’ve found or just the bottom line and what I would recommend?” Again, this type of presentation strengthens the clinician’s position with the patient as a partner or ally, while also assessing the patients desire for more information and details as to possible solutions.
Step 3: Check on the importance of change
- Begin by reviewing the results of the hearing loss impact questionnaire. Revisiting the patient’s self-assessment will remind them of the issues they are having and help gauge how willing they are to actually make a change. Something as simple as asking the patient how important it is for them to make a change on a scale from 1 to 10 can help steer the conversation. If they indicate a very low number, for example, discuss the potential outcomes for action vs. inaction.
Step 4. Assess the patient’s belief in their ability to succeed
- Assess the belief to succeed only when the patient indicates importance for change is high. Reaffirm the patient’s desire to improve their communication and ask them if they would be willing to follow your recommendation if it included the use of hearing aids. This will allow you to address any objections the patient may have to amplification and, hopefully, get them on the path to better hearing.
Engaging Your Patients
Further resources and discussion on motivational engagement in the hearing clinic can be found in Counseling-Infused Audiologic Care {{5}}[[5]]Clark, J.G. & English, K.E. (2014). Counseling-infused audiologic care. Boston: Pearson Education.[[5]] and as a side benefit, the American Board of Audiology (ABA) has arranged to offer up to .7 CEUs through the American Academy of Audiology tied to directly to reading the book and taking a series of multiple choice exams.
Free tools and CEUs on the use of motivational engagement are also available through the Ida Institute.
_
*Featured image courtesy upstart.bizjournals.com






