Jennifer Shinn, PhD, Professor and Chief of Audiology, Department of Otolaryngology, University of Kentucky Medical Center
Trey Cline, AuD, Clinical Audiologist, Department of Otolaryngology, University of Kentucky Medical Center
Introduction:
A significant part of our clinical practice is evaluating and managing patients with auditory processing disorders (APD). All too often adults are overlooked when it comes to evaluation of the central auditory system because these evaluations are primarily performed in the pediatric population. In addition, patients who present with normal peripheral hearing sensitivity may be told that there is no hearing loss, but clinicians fail to evaluate central auditory function. The majority of the patients seen in our clinic who are evaluated for APD are in fact adults. Adults with auditory complaints in spite of normal peripheral hearing sensitivity are interesting and sometimes challenging cases. The purpose of this article is to present the reader with a case example of an adult patient who recently presented in our office with auditory complaints and was subsequently diagnosed with an auditory processing disorder. We will review the tests results, management approaches and outcomes of this case.
Case:
This is the case of a 39-year-old male who was referred by a speech-language pathologist (SLP) due to concerns for an auditory processing disorder. He had not actually been evaluated by the SLP. In a phone consultation with the patient, the SLP felt that an APD evaluation would be a more appropriate first step based on his history and thus referred him to our clinic.
With respect to his auditory history, he reported longstanding difficulty hearing. In particular, he reported significant difficulty understanding speech in the presence of background noise and when people are speaking quickly. He indicated no concerns regarding hearing sensitivity (an important distinction to make during a case history). Interestingly, he is a recreational pilot with the goal of obtaining his instrument reading certification. This requires him to rely heavily on auditory information with little visual cues. He reported having difficulty with this as traffic control often communicates quickly and he is unable to always understand what has been said. As we have observed with many patients during the pandemic, he also noted difficulty hearing due to masks (which have built-in filtering) and an inability to rely on visual cues. He reported that in general his rate of auditory processing is slower than most individuals. He and his wife both reported significant difficulties following multistep directions. While he did admit to a history of noise exposure, he reported that he has consistently used hearing protection. No significant otologic history was reported.
Other relevant history includes that he was diagnosed with ADHD during elementary school and was on Ritalin for a number of years. He discontinued use of pharmacological management of his ADHD in high school. He also received speech therapy as a child for articulation deficits (it has been our experience that some children with articulation deficits present with APD). He also had significant difficulty with reading comprehension, learning music and foreign languages. With effort and tutors, he has done well academically and holds a Masters degree.
The patient was also asked to complete the Speech, Spatial and Qualities of Hearing Scale (SSQ) (Gatehouse and Noble, 2004). The SSQ is self-report questionnaire designed to evaluate hearing difficulties across the domains of speech, spatial hearing, qualities of hearing. We ask that all adult patients complete the questionnaire at the time of their evaluation.
This patient was initially evaluated with a comprehensive audiological evaluation which demonstrated normal peripheral hearing sensitivity from 250-3000 Hz with a mild, symmetric sensorineural hearing loss for the remaining frequencies. Speech audiometry demonstrated excellent word recognition bilaterally (100% right ear, 90% left ear).
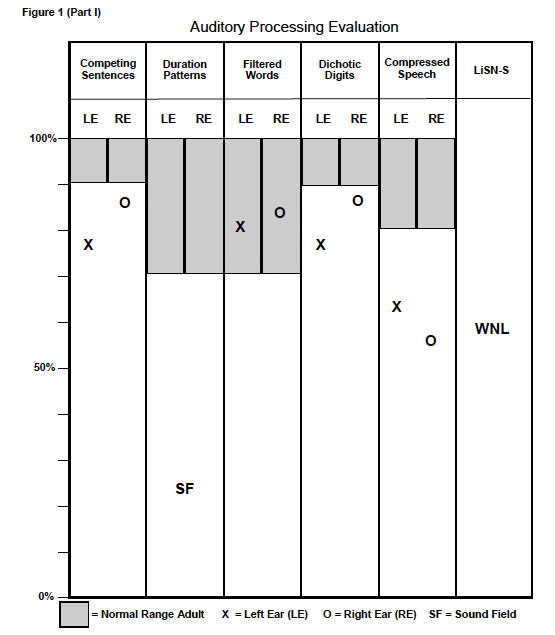
Following the audiological evaluation, the patient underwent an auditory processing evaluation, which included the following: the Dichotic Digits (DDT), Duration Pattern (DPT), Filtered Words (FWT), Competing Sentences (CS), Compressed Speech (CST) and Listening in Spatialized Noise (LiSN-S) tests. As seen in Figure 1, performance was abnormal for all tests with the exception of FWT and LiSN-S. Based on these test results, the patient was diagnosed with an auditory processing deficit in the areas of binaural integration, binaural separation, temporal processing, and rapidly presented speech.
The results and recommendations were discussed with the patient and wife. Given the left ear deficit on both binaural separation and integration tasks, it was recommended that the patient return for dichotic interaural intensity difference (DIID) therap. In addition, in our experience, patients who present with APD also find significant benefit from the use of amplification (this will be discussed further in Part II of this article). The patient was very eager to proceed, highly motivated and initiated DIID therapy shortly after his evaluation.
Dichotic Interaural Intensity Difference (DIID) Training
For the reader who is unfamiliar with DIID therapy, this is a direct form of formal auditory therapy designed for patients with binaural integration and/or separation deficits. DIID therapy was first introduced by Drs. Musiek and Schochat (1998) with their work in individuals with known lesions of the corpus callosum. The underlying concept of DIID therapy actually comes from the physical therapy rehabilitation literature focused on constraint-induced therapy (CIT). Constraint-induced therapy is used in stroke patients to improve motor function in weakened limbs. The stronger limb is immobilized (constrained) and therapy requires forced use of the paretic/weakened limb to improve function (Taub et al., 1993).
Previous research has demonstrated the effectiveness of DIID therapy. In children, Moncrieff and Wertz (2008) demonstrated improvements in dichotic listening deficits after intensive rehabilitation using digits and words as stimuli. Participants also demonstrated improved word recognition and language comprehension following the training at which the authors suggested that training might help to facilitate language skills in the pediatric population. In a case study by McCullagh and Palmer (2017), the researchers demonstrated the effectiveness of DIID therapy in an adult who had suffered a left cerebral vascular accident and presented with a binaural integration deficit. More recently, we have published data that also supports significant improvement in patients and anatomical changes in participants who have undergone DIID therapy (Cline et al., 2021).
The DIID procedure is performed by decreasing the intensity level of the stimulus presented to the better ear and therefore, forcing the weaker ear to become the primary auditory pathway in order to understand the stimulus. By decreasing the presentation level to the better ear, it is hypothesized that the ipsilateral auditory pathways to the poorer ear are released from suppression and this will allow more neural substrate to contribute to the poorer ear performance during training. The ultimate goal of the training is for both ears to perform normally on dichotic listening tasks at equal presentation levels (Musiek, Weihing and Lau, 2008).
In part one of this two part series, we have laid out an interesting, but not uncommon case of a patient seen in our clinic. He demonstrated classic APD complaints of difficulty hearing in background noise and understanding speech from people who are speaking quickly. He acknowledges difficulty following multistep directions and that he feels as if it takes him longer to process auditory information. He was diagnosed with an auditory processing deficit through a formal APD evaluation with specific difficulties in binaural integration, binaural separation, temporal processing, and rapidly presented speech. Additionally, we have introduced the formal DIID therapy for deficits with binaural integration and separation and some of the research supporting its use. In part two of this series, we will discuss the results of his DIID therapy as well as other management strategies used to address his APD. Finally, we will discuss the patient’s perceptual improvements following intervention.
References
Cline T, Colgrove N, Bush M, Lee J, Powell D, Anderson A, Weihing J, Musiek F, Shinn J. (2021). Behavioral and Hemodynamic Changes Following Dichotic Training in Patients with Neurological Deficits of the Central Auditory Nervous System: A Case Series. J Am Acad Audiol 32(1): 45-53.
Gatehouse S, Noble W. (2004). The Speech, Spatial and Qualities of Hearing Scale (SSQ). Int J Audiol 43(2): 85-99.
McCullagh J, Palmer SB. (2017) The effects of auditory training on dichotic listening: a neurological case study. Hearing Balance Commun 15(1): 30-37.
Moncrieff DW, Wertz D. (2008) Auditory rehabilitation for interaural asymmetry: Preliminary evidence of improved dichotic listening performance following intensive training. Int J Audiol 47: 84-97.
Musiek FE, Weihing J, Lau C. (2008) Dichotic interaural intensity difference (DIID) training: a review of existing research and future directions. J Acad Rehabil Audiol XLI: 51-65.
Musiek FE, Schochat E. (1998) Auditory training and central auditory processing disorders. Semin Hear 19(4): 357-365.
Taub E, Miller NE, Novack TA, Cook EW 3rd, Fleming WC, Nepomuceno CS, Connell JS, Crago JE. (1993). Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil 74(4): 347-354.
Weihing J, Musiek FE. (2014) Dichotic interaural intensity difference (DIID) training. In: Chermak GD and Musiek FE, ed. Handbook of Central Auditory Processing Disorder: Volume ll Comprehensive Intervention. San Diego: Plural Publishing, 225-242.