Neurosoft Bioelectronics is leading the way in the development of sophisticated soft implantable electrodes designed to interact with the brain and address severe neurological disorders. In this week’s discussion, host Bob Traynor engages in a conversation with CEO Nicolas Vachicouras, delving into the company’s pioneering initiatives to create an implantable brain interface device aimed at treating severe tinnitus.
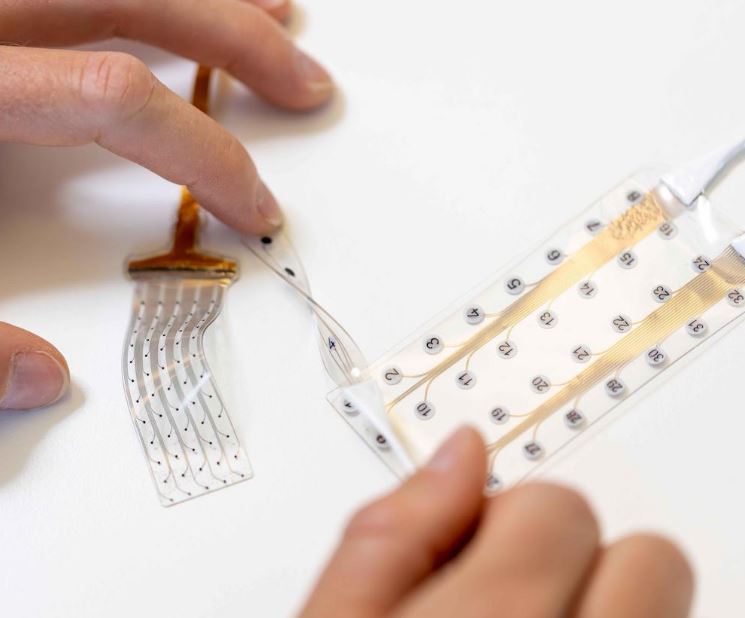
The technology employs ultra-thin, flexible electrodes capable of both recording brain activity and delivering personalized electrical stimulation patterns, guided by AI algorithms. The overarching objective is to regulate hyperactive networks associated with conditions such as tinnitus through a closed-loop system.
 Human trials have substantiated the safety and effectiveness of these electrodes in recording brain activity. Neurosoft’s strategic roadmap includes the launch of a product for epilepsy and the initiation of a specialized feasibility study for treating severe tinnitus. With a minimally invasive implantation procedure, this technology holds the potential to offer long-term relief for individuals grappling with chronic tinnitus. Neurosoft envisions introducing new treatment options within 4-5 years, pending further development and regulatory approval.
Human trials have substantiated the safety and effectiveness of these electrodes in recording brain activity. Neurosoft’s strategic roadmap includes the launch of a product for epilepsy and the initiation of a specialized feasibility study for treating severe tinnitus. With a minimally invasive implantation procedure, this technology holds the potential to offer long-term relief for individuals grappling with chronic tinnitus. Neurosoft envisions introducing new treatment options within 4-5 years, pending further development and regulatory approval.
More information on the technology can be found on the company’s website
Full Episode Transcript
Welcome to This Week in Hearing. Hello, I’m Bob Traynor, your host for this exciting episode about a new European orientation to severe tinnitus by a company called Neurosoft Bioelectronics, a company that uses AI and machine learning. And some of the things we’re on the verge of here in our profession for the treatment of severe tinnitus. Today, my guest is Nicolas Vachicouras, who is the CEO of Neurosoft Bioelectronics. And thanks for being with us today, Nicolas, and we’re really excited to hear about your new product that may be able to work with us and. Are patients that do have severe tinnitus. Nice to meet you, Bob, and thank you for having me here today. Well, so the first thing I like to do with these sessions, Nicolas, is, you know, how did you get into working with tinnitus patients, and how did you get into this area where you’ve come across this Neurosoft Bioelectronic system? Yeah. So my background is actually in microelectronics and nanosystems. So I’m more like engineer and background. I did my studies in Switzerland. And actually, during my studies, one of the first projects I did as a PhD in our field was around the hearing, actually. And I was in Boston for one year where I did my master’s thesis. It was still about bioelectronics, and I’ll tell you more about it, but it was in a specific case of what we call. Auditory brainstem implants. So these were device to provide hearing sensations to patients who are not candidates for cochlear implants. So it was not tinnitus back then, it was more on the hearing but it was the first and the main project I did during my PhD so it was actually at Massachussetts Eye and ear infirmary with ENT and neurotologists. So that’s how I got into the let’s say ENT field and when we started the company and I’ll tell you more about it but we’re developing these brain interfaces to record and stimulate nervous system and we were looking into different indications that we could help. And during that time there was a study ongoing at EPFL. So the university that was sponsored also by the … foundation here in Geneva that was about severe tinnitus. So they were looking into functional MRI into very severe cases and trying to look at the brain of these patients. So we got curious about severe tinnitus. We looked into it and we realized there was a huge unmet clinic need. And by talking to some patient associations, patients, ENTs, neurotologists, we realize that there is potentially something that we can do about it with our technology. Fabulous. And we all know that some of the most innovative things come from individuals with different training than we have in working with our patients. And we put all that together with what we know about the patients and what some of our new colleagues know about all these other things that we never studied, ever. So why hasn’t there been a treatment for severe tinnitus, or what we often call bothersome, sustained tinnitus? And again, and we may see one of these patients every couple of years, but when we see this one, it just drives us nuts. Try to figure out what we’re going to do, how we’re going to take care of those guys and what kinds of things they need to facilitate a movement back into the normal situation. Yeah, that’s a good question. So as you probably know, tinnitus in general with all considerations is a huge problem worldwide. I think it’s around 15-14% of the world population and as you mentioned we’re focusing on these very small but still large subset of patients who are very severe, so chronic and debilitating which is about 120,000,000 people worldwide. And what I’m learning also as I got into this is that it’s actually a very heterogeneous population. So you have very different causes for the tinnitus. It could be viral, it could be noise exposure which I would say is the most common and we’ve even seen COVID has increased tinnitus incidence. So there’s different things. So I think that’s one of the reasons is that it’s not only one disease or disorder, it’s really some. That can be caused by multiple aspects. So obviously you’re not going to treat patients the same way depending on what’s the root cause. And I think the other bigger problem, as you probably know, is that there’s limited understanding of the precise mechanism that causes tinnitus. So there was also a lot of work actually, that was done more recently that guided us towards what we believe could be a good solution, but it’s still something that is relatively not understood. And I think the last element is that it’s a very subjective disorder, so it’s very hard to measure. You probably are aware of all these scales and try to ask patients how they feel about it. So when you don’t have a very precise quantitative method to assess it, it’s hard to know if whatever you’re trying is actually having a clinical impact or not. So I think these are the different elements that make it that there’s today no treatment. Okay, well, yeah, and that’s always been an issue. The subjectiveness of the tinnitus has always been an issue. Whether it’s something that was created by an accident or whether it was something that was created by certain kinds of noise exposure or other kinds of things, it’s always been an issue. So what kind of a product are you presenting to those of us that would be treating tinnitus patients? Nicolas- so it’s still early stage project, but as I mentioned earlier, I got interested in the field of what we call bioelectronic interfaces. So these are implantable brain devices that can interact with the human brain. So these are electrodes that can either read or write into the brain so they can be used to record or stimulate electrically. And that’s something that is not new. I mean, it has been used actually to help patients with Parkinson’s disease order to remove symptoms. It has been helped for patients who have spinal cord back pain to stimulate the spinal cord and relieve the pain, or cochlear implants, I think are a very. Good example of how electricity has been able to provide auditory sensations to patients. So this is the field where we’re at. And at Neurosoft, we developed a new type of electrodes that are much thinner, they are much softer, so they are actually much safer to use and they are able to record and stimulate the human brain. And so based on some of the more recent studies that were performed, tinnitus understanding the mechanism of action, what we have realized is that in a lot of these severe cases, this is not only a problem in the ear, but there’s actually underlying issues within the brain where you have hyperactive networks. And again, this can change across patients, but there’s really in a lot of these patients an issue at the level of brain. So the idea is to try to the same way people are able to stimulate the brain to remove symptoms for Parkinson’s, to try to rechange these pathological networks through electrical stimulation and recording to help. These patients. So that’s in a nutshell what we’re trying to do. Okay, so now you’ve been doing some human testing with your products recently, I guess. And can you tell us more about that and what it really means for the efforts of working with severe tinnitus patients? Yeah, so very good question. So obviously, we are working with very innovative and new technologies. So the first thing we wanted to do is to demonstrate just the ability of our devices to function within the human brain. So, for example, to record human activity. So until now, we’ve done a lot of animal testing to demonstrate the safety. And we arrived this summer at a point where we were ready to test it in humans. So we did it in a very different condition. It was for epilepsy patients or brain tumor patients where we have, let’s say, easier access to the brain during surgery. And we were able within a few patients, four so far, to really just test the ability of our device to record. From the human brain in a realistic environment. So for us, it was a very meaningful milestone just to demonstrate it was not about tinnitus, this one, but really about the safety and the effectiveness of our device to interface with the brain. So that was really one of the first milestones before we go further towards tinnitus. So what’s so special about this particular electrode. I mean, I put electrodes on ABR people all the time, and back in the old days we did ENG and we put electrodes around the eyes. What’s so special about your particular electrode that makes it different from the electrodes that most of us know and love because of our assessment techniques? Yeah, that’s a good question. So the motivation behind our work comes from the observation that the brain and neural tissues are very soft, so you can think of it like spanacotta or tofu. And the problem is that until recently, the best way we had to interface with these tissues. Were with very rigid electronics like hard metals and they were not very well accepted by the body. So we had what we call foreign body reaction where you basically have scarring. These devices push the brain, they can compress it, they can damage it. So they were not great interfaces and so this motivated our work at the university and now with the company to really develop what we call soft bioeletronic interfaces. So material that are much thinner, much more flexible, actually stretchable to make them in general safer but also to allow us to access brain regions that you’d otherwise not be able to because it would be too risky with other devices. So this is really the main element. It’s really about having a safer interface that has a bigger chance of surviving what we call the very harsh environment of the brain because you have a lot of liquids, it’s in movement, it’s soft, you have tissues, there’s a lot of happening. So that’s the first main element. The other one is. We have sensors on these electrodes, so these electrodes can record and stimulate. And today, a lot of these electrodes are relatively large. So think of a TV screen with a few pixels, you won’t get a very good image of what you’re looking at. So we are able to have lot smaller and much closer together electrodes to get a better picture of the brain and on the opposite direction, if you’re stimulating, having smaller electrodes allows to stimulate more precisely and to ensure you’re not stimulating parts of the brain that you do not want to, which might cause secondary effects. So these are really the two elements, smaller electrodes and softer materials. Wow. So we have been hearing all kinds of stuff about AI. Machine learning has been around for a while, but probably not in things that we do very much. So, can you tell me how AI and machine learning and these kinds of things work within your solution. Yeah, no that’s a very good question. So for us, until recently, if we look at the, in general, neuromodulation, as we call it, it’s always been done what we call open loop, meaning that the device is just stimulating the same region constantly. And that’s what it does. And one of the big trends today in general, and I think this will apply very, very well to tinnitus, is to do what we call closed loop. So this means that you’re getting feedback back. So you’re not only stimulating blindly, but you’re trying to understand what’s happening when you stimulate and try to use this information to tailor the stimulation. So our goal is to have a device that can both stimulate electrically but also record the activity of the brain, understand what is happening in terms of, we can ideally find activity that is correlated to the level of tinnitus. See can we reduce it? If so, use this information to better tailor the stimulation for every single patient. And so this is where AI and machine learning is very, very useful because you can gather a lot of data, because imagine you have tens or maybe hundreds of electrodes that are recording continuously brain data that is very hard to interpret. This is where AI and machine learning can be a very powerful tool to interpret this information and to really tailor the way we will stimulate and eventually treat the patients, hopefully. So that’s how we’re using it within this closed loop system. Okay. Now, I don’t know. Most of my tinnitus patients aren’t going to really decide they want to go have surgery. Brain surgeries, although they’re much better than they were 30, 40 years ago, they’re still a little risky these days. And how does the Neurosoft product help make that a little bit safer for each and every patient that we would see? Yeah, it’s a very fair question. And so, as I mentioned just earlier, the fact that we’re using these softer materials. Is already a great way to de-risk a lot of the risk associated with these devices, and I think that plays an important element. And this is also why we’re doing all these preliminary studies to demonstrate the safety of these electrodes. Now, one thing that we’re quite excited about is that indeed, the surgical approach to date, to implant some of these devices can require a big opening in the skull. And so trying to leverage the fact that our devices are made of very stretchable materials. So think of them like a rubber, and what’s nice is that you can actually fold it without breaking it and unfold it onto the surface of the brain through a small hole or a smaller opening. And so this is something that we’re trying to leverage because we’re in a unique position, thanks to the materials we’re using, to be able to do this folding on folding without damaging the electrodes and allowing us to do what we call minimally invasive approach. And so this is really, for us, one of the elements we try to leverage. Make this also more appealing. So it’s not going to be like acoustic neuromas surgery or anything like that. It’s going to be more like a very focused kind of an area. Where do the electrodes go? Do they go on Heschl’s gyrus area? Do they go in different other parts of the brain? So I guess that’s kind of two questions for in there. Yeah, it’s a good question, and it’s something that we’re currently discussing exactly what and where we’ll be stimulating. And this is something we’re also doing with some of our advisors who have a lot more experience than us. But indeed, parts of the brain that we’re interested in are it’s all cortex. So surface of the brain, and indeed one of them is auditory cortex. And we’re also looking at the Heschl’s gyrus in terms of access to other regions there. Okay. And I assume that you were mentioning that you had some research. At Mass Eye & Ear and some of the other places that had been going on. And you also, I think, said something about there were some animal research first and then showing that it worked and it did some things and then moved on into the human kind of areas. Do you see any ethical kinds of risks with this brain technology that as we move forward with AI and machine learning and surgery for tinnitus and things like that, it’s like, whoa, that’s quite different than what we’ve been using over the last number of years with our tinnitus patients. No, it’s a great question. And people are talking a lot about what they call neuroethics. So it’s an important topic that we are faced with. So in some of the concerns that I can think about with these devices within tinnitus or in general, are, well, everything that has to do with privacy, consent. And also, obviously, potential misuse of these devices. So obviously, one big part of what we’re doing is when we are doing our clinical studies for now, for epilepsy, and we’ll start hopefully soon for tinnitus is to make sure that we ensure data privacy and ethical enrollment of the patients, that they’re well informed. I think that’s definitely something very important for us. And for potential misuse, that’s a bigger risk. Obviously, we’ll try our best to make sure that device cannot be used outside of its intended use, which is to treat patients. And we all stay aware of what’s happening, what are the potentials of these technologies? But for now, we think there is a lot more to gain with these devices, not only for tinnitus, actually, but for a lot of neurological disorders. And so these are some of the topics that we’re keeping in mind and trying to think about as we’re developing these devices. Okay. Yeah. I would think there’d be some ethical things that you’d have to kind of work through. Not necessarily. Then it’s unethical or anything. It’s just that it is one of those things that when you have a new kind of a system, you always have to work through some of these esoteric types of questions that go along with it in ethics and that type of. So from where you are today, Nicolas, what are the next steps for Neurosoft as a company and as a technology and that type of thing? Yeah. So, as you mentioned, we started our first trials over the summer in Texas. And in the context of epilepsy, and concretely now, we’re currently fundraising. And with this fundraise, we have two big objectives. The first one is to bring to market our first electrode. For epilepsy. And that’s also, even though it’s for epilepsy, I think it’s going to be a great way to also de-risk not only technologically but also from a regulatory perspective with respect to the FDA, our device. And then our big goal in the upcoming, I would say year or so is to do a feasibility study for severe tinnitus. So our goal is to start with a first smaller trial with few patients just to test the feasibility of this, to better understand what works, what doesn’t, to tune exactly how we’re going to stimulate. And I think that will be one of the big milestones we want to reach as soon as possible. So how long do you think it’s going to be before, if I’m seeing severe tinnitus patients in the severe tennis patient in a clinic, how long is it going to before I call up my Neursoft Rep and the ENT and figure out a way to fix that person? It’s a good. Question. It’s a hard one just to give you an idea. I mean it took us about four years and a half to go from our research environment to first in epilepsy so we’ve done definitely some progress. I still think it will require a bit of work and one of the reasons is even if we had a system that was working at least for regulatory approval you need data that is long term. So I would say at least one year follow up. So just because of that things are going to take time. I don’t have a definite timeline but I think four or five years is kind of what we’re aiming for. I think that’s the timeline to develop the technology, do our feasibility study, do what we call a pivotal study and get regulatory approval. Wow. Yeah. Now is this something be appropriate for hyperacusis as well? It’s a good question and we don’t know yet. It’s something that we’re going to monitor because we know that there’s. In some of these patients. So I cannot answer. I’m not completely sure. It’s definitely something that we want to monitor because indeed, we might be surprised and we might see benefits in places that we had not thought about at the beginning. Yeah. Wow. I’m interested because having always been kind of involved with tinnitus for such a long time, the idea, first of all, that you could do something about it in the late 70s was like, wow. Then we found different things that worked for different patients. But the severe tinnitus patient, the severe, bothersome individual, has always escaped us, and usually it’s CBT or one of these other treatments that are out there, but they’re still not as efficient and effective as we would like. I really appreciate. Appreciate your coming into our discussion here at this week in hearing Nicolas and presenting what is a possible beginning of the use of AI and machine learning. And all of this is to colleagues out there. A lot of this is coming from individuals with huge backgrounds in other areas that bring their expertise into the problems that we see in the clinic every day. Thanks again for being with us, Nicolas, and we’ll look forward to seeing more of you and your product as it develops and so on. So please come back to us here at This Week in Hearing. And as the updates come out, we’ll update our clinical group about these things. Thank you very much. So my guest today has been Nicolas Vachicouras. CEO of Neurosoft Bioelectronics, a new company, a European company, but it’s got some US interactions as well. It sounds like that is trying to use AI and machine learning in the treatment of tinnitus. Be with us next time for This Week in Hearing
Be sure to subscribe to the TWIH YouTube channel for the latest episodes each week, and follow This Week in Hearing on LinkedIn and Twitter.
Prefer to listen on the go? Tune into the TWIH Podcast on your favorite podcast streaming service, including Apple, Spotify, Google and more.
About the Panel
 Nicolas Vachicouras, PhD, is the CEO & Co-Founder of Neurosoft Bioelectronics. He holds a MSc and PhD degree in micro-electronics from EPFL. He has eight years of experience working in the field of neuroprosthetics. Nicolas holds a Certificate of Advanced Studies in the management of medtech ventures.
Nicolas Vachicouras, PhD, is the CEO & Co-Founder of Neurosoft Bioelectronics. He holds a MSc and PhD degree in micro-electronics from EPFL. He has eight years of experience working in the field of neuroprosthetics. Nicolas holds a Certificate of Advanced Studies in the management of medtech ventures.
 Robert M. Traynor, Ed.D., is a hearing industry consultant, trainer, professor, conference speaker, practice manager and author. He has decades of experience teaching courses and training clinicians within the field of audiology with specific emphasis in hearing and tinnitus rehabilitation. He serves as Adjunct Faculty in Audiology at the University of Florida, University of Northern Colorado, University of Colorado and The University of Arkansas for Medical Sciences.
Robert M. Traynor, Ed.D., is a hearing industry consultant, trainer, professor, conference speaker, practice manager and author. He has decades of experience teaching courses and training clinicians within the field of audiology with specific emphasis in hearing and tinnitus rehabilitation. He serves as Adjunct Faculty in Audiology at the University of Florida, University of Northern Colorado, University of Colorado and The University of Arkansas for Medical Sciences.