Accommodating the OTC Hearing Aid Discussion: Hearing Screening in the Absence of Audiometry – Part 2
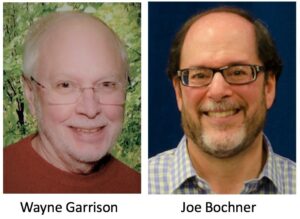
by Wayne M. Garrison* and Joseph H. Bochner**
 This is the second of a two-part series on an evaluated option to hearing level identification to fit OTC hearing aids in the absence of audiometry. Part 1 introduced an online hearing level identification test, the NSRT (NTID Speech Recognition Test)1 that could be used to circumvent the belief by some that a pure-tone audiogram is critical to any hearing aid fitting, much less for OTC hearing aid sales. Data obtained from the NSRT® testing experience are used to construct a pseudo audiogram. We report that, when predicted hearing thresholds are compared with conventional, clinical pure-tone measures, the sensitivity and specificity of the NSRT® screening measure have been found to be 95% and 87%, respectively; diagnostic accuracy is 91%2. These statistics reinforce the argument for OTC hearing aid sales suggesting that, in addition to self-fitting, self-assessment may be a viable way to manage the market of those individuals not served by current audiological practice.
This is the second of a two-part series on an evaluated option to hearing level identification to fit OTC hearing aids in the absence of audiometry. Part 1 introduced an online hearing level identification test, the NSRT (NTID Speech Recognition Test)1 that could be used to circumvent the belief by some that a pure-tone audiogram is critical to any hearing aid fitting, much less for OTC hearing aid sales. Data obtained from the NSRT® testing experience are used to construct a pseudo audiogram. We report that, when predicted hearing thresholds are compared with conventional, clinical pure-tone measures, the sensitivity and specificity of the NSRT® screening measure have been found to be 95% and 87%, respectively; diagnostic accuracy is 91%2. These statistics reinforce the argument for OTC hearing aid sales suggesting that, in addition to self-fitting, self-assessment may be a viable way to manage the market of those individuals not served by current audiological practice.
The use of the term “hearing screening” in this article is not to be confused with hearing screening that uses pure-tone signals.
Self-Administered Automated Speech-Based Hearing Screening Test (NSRT®)
Information reports and interpretation resulting from NSRT self-evaluation are provided in this post. Readers are encouraged to take this online test at https://apps.ntid.rit.edu/NSRT/ to more fully understand and appreciate this self-test of hearing.
Output Displays of the Online Screening
After completing an NSRT® adaptive testing session, respondents have the option to view a variety of tabular/graphical displays illustrating their hearing screening results. Before any testing results are provided, however, NSRT® data are subjected to a statistical, “plausibility” analysis. The overwhelming majority of test records examined at this point have been found to be valid. In a small number of cases, however, we have observed enough “noise” within a test record to preclude the output of screening results, insofar as the accuracy of these same results is questionable. Questionable test records are generally the result of carelessness, inattention or otherwise unintended human behavior during a testing session. Individuals whose test records are flagged as questionable are invited to retake the test.
The simplest of the displays that can be output following a hearing screening test is shown in Figure 1. For many individuals, this simple summary of their performance on the screening measure will be sufficient. Moving from left to right across the tabs shown moves the respondent to other diagnostic displays.
The respondent’s hearing screening test score expressed on a scale that extends from 0 – 100 is illustrated in Figure 2. The NSRT® score corresponds roughly to the percentage of speech that one is able to recognize in everyday listening situations. A confidence interval associated with the score is also shown. It represents the range of scores within which we would expect to find one’s “true” NSRT® score 95% of the time on repeated testing, under the same testing circumstances. The NSRT® score may be considered a functional measure of overall hearing sensitivity. Scores obtained in noise will be lower than those obtained in quiet. Note, however, that the NSRT® is only one piece of information that is used in assessing a respondent’s overall level of hearing sensitivity.
A screenshot of the tabular display available to respondents that statistically combines the information available via the NSRT® testing experience with other self-report data (elaborated at the left of the screen capture) to produce an audiogram (for the better ear), is shown in Figure 3. This pseudo audiogram has been found to conform closely to the audiogram that would be obtained under more controlled, clinical conditions. The NSRT® application does not currently provide threshold data for left and right ears separately since the auditory stimuli usually are delivered to both ears. The next version of the NSRT will allow the user to test each ear separately.
In the “Application to Speech Sounds” tab, we use the NSRT® score in quiet to illustrate the probability that a respondent is able to recognize specific phonetic categories of speech. The “History” tab enables respondents who have tested on more than one occasion or under different testing conditions (i.e., quiet vs. noise) to compare/contrast their pseudo audiograms in graphical format.
Concluding Comments
In its 2015 report, the President’s Council of Advisors on Science and Technology support the claim that hearing loss in an aging population is now a “substantial national problem,” citing cost as the largest barrier to hearing technology access by individuals who could benefit from amplification, simultaneously advocating changes in FDA regulations that include disruptive improvements in both the assessment and treatment of hearing loss.
On the treatment side of the argument, the OTC Hearing Aid Act of 2017 is now pending legislative action.
On the assessment side of the argument, R/D efforts described herein suggest that self-testing may also hold a place in managing the market of those individuals who are not otherwise served by professionals.
Does the move to self-assessment and OTC hearing aid sales diminish the role of audiologists in the delivery of hearing healthcare? Not at all! It actually sharpens and focuses their work with individuals who fall outside the range of mild to moderate hearing loss.
We invite commentary on our work.
References
- Bochner, J. H., Garrison, W. M. and Doherty, K. A. (2015). The NTID Speech Recognition Test: NSRT®. International Journal of Audiology, 54, 490-498.
- Garrison, W. M. and Bochner, J. H. (2015). Applications of the NTID Speech Recognition Test (NSRT®). International Journal of Audiology, 54, 828-837.
*Dr. Wayne Garrison is a Research Professor at the National Technical Institute for the Deaf on the Rochester Institute of Technology campus in Rochester, New York. He is a psychologist by training, with a broad range of R/D experience in statistics, psychometrics and software design.
**Joe Bochner is a professor and department chair at RIT/NTID. He has been involved in the language sciences, deafness and higher education for four decades, conducting research on the acquisition of English language and literacy skills, speech perception and production, and American Sign Language.











Of course, those who’ve actually researched the market up close and personally for decades know that cost is NOT at the top of the list of barriers to hearing health care. It’s barely at the bottom of the list, and with every nook and cranny of the US population being served with the finest and most up to date equipment, instrumentation, and expertise, access is not even on the list. You can get quality, basic hearing aids with full services for less than $600 just about everywhere.
The PCAST Committee, I’m sorry to say, assumed much and understands little about the hearing aid market. Denial and lack of internal reference are at the top of the list of reasons most people wait 15-20 years before getting hearing aids.
Even so, the fact that market penetration in the mild and moderate loss categories has about doubled over the last decade with the advent of digital RIC instruments has been lost on virtually on every critic of our industry.
Now, we are about to lose the most important consumer protections (FDA red flags and medical clearance for potentially life threatening conditions that cannot be self assessed) and the unsuspecting consumer is about to be at the mercy of untrained and unlicensed dispenser and unscrupulous corporate players who are chomping at the bit to ignore what it really takes to make a hearing aid future and programmed with meaningful outcomes. Ignorance and greed prevail and the hearing impaired are the losers most of all. A hearing aud at any price that dies not involve a fully trained and licensed professional costs too much at any price.
Apologize for Siri typos in above but meaning should be clear.
Hearing loss occurs as a result of some form of pathology for people who are not yet old. Such people will need counseling to aid them in the future years, and includes the need to respect their hearing loss, as one with unintended consequences like cognitive impairments. Hence it would be in their best interests to wear the aids under professional advice. In any case I don’t see increase in the use of hearing aids as each individual has to go through a “denial phase”, before seeking help. There could be a population that has SSNHL, and they will definitely need medical intervention. This needs to be advertised.