In the Fall of 2017, I experienced an episode of acute right vestibular neuritis (VN). I joke that I likely have the most well documented case of VN on record. I am often the first live patient most of our students test as I am a willing example of “abnormal.”
Seven years later, my permanent vestibular dysfunction has faded to the background, and rarely does anyone see any evidence of the lingering issues that many VN patients suffer. I have adjusted my lifestyle accordingly, but since I am most impacted by visual instability with rapid head movements and balance in challenging environments, it seems like I am griping about “first world problems” when I note that I cannot play tennis or paddleboard as well as I did prior to the injury. Lack of sympathy duly noted.
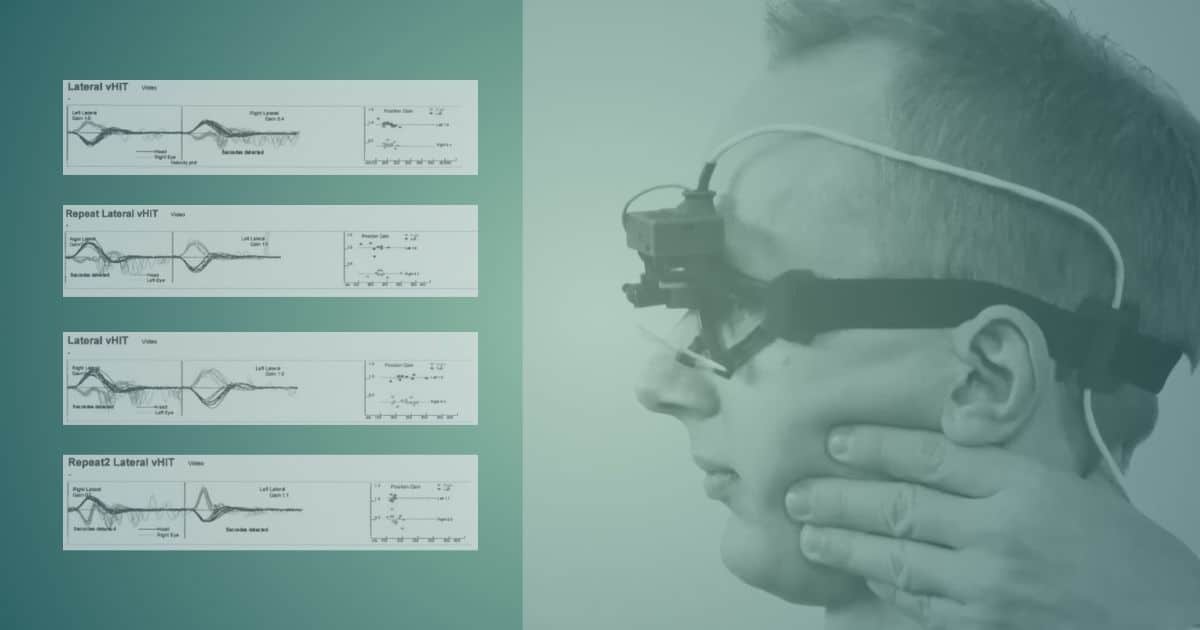
The compensation process, while not linear, has both subjective and objective components. I have tracked my progress through both rotational chair and lateral vHIT testing. Below are my vHIT exams over a four year period:
ACUTE STAGE
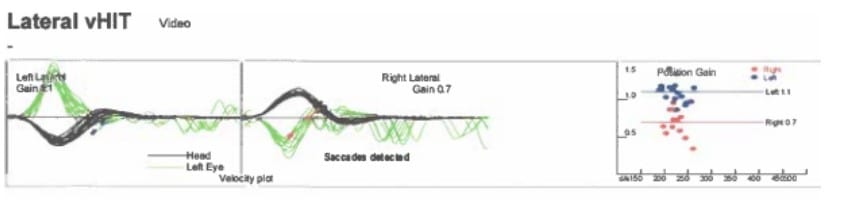
The first vHIT tracing below was obtained approximately 48 hours following onset of acute prolonged vertigo. A spontaneous, left-beating, horizontal nystagmus measuring 13 degrees/ slow phase velocity (SPV) in darkness was present at the time.
48 hours
Symptomatically, the sensation of vertigo was ongoing with gradual subjective decrease over four to five days. I could walk with a cane after 48 hours. By day five I was comfortable while sitting still, and could fixate enough to read or watch TV. At day seven, I returned for follow up testing.
The spontaneous nystagmus had reduced to 4 degrees/SPV. The vHIT below demonstrated complete disorganization of corrective overt saccades with very low gain in the rightward direction.
7 days
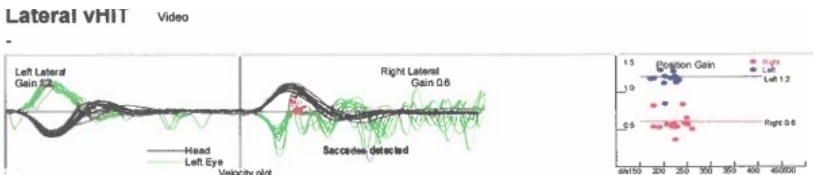
One week later, I was over the acute stage, but still had 4 degree /SPV spontaneous nystagmus. I had not started doing any type of rehab and was basically just resting. The vHIT below shows some organized covert saccades, followed by disorganized overt saccades.
14 days
I was still not driving but began VOR and balance exercises. I was back at work and quite unsteady but functional.
CHRONIC STAGE
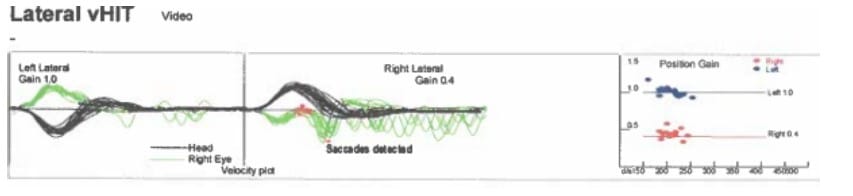
At 30 days, we started to see some development of covert saccades. You can also see below that most of the overt saccades are occurring closer to the cessation of head movement.
*Note: The tracings from this point forward have the right ear on the left side of the graph, whereas the right ear was shown on the right side of the graph in earlier tests.
30 days
After 90 days, you can see below that the covert saccades are beginning to overlap, meaning that my eyes are spending less time off the target when moving quickly to the right because I have learned to start a corrective eye movement while my head is still in motion. You will note that the gain measurements do not change significantly over time as I suffered a profound loss of vestibular function with no recovery on the right side.
These improvements noted are strictly the result of vestibular compensation with no recovery of labyrinthine function. By this time, I was driving but still uncomfortable in unfamiliar areas where I had to be able to read road signs while driving.
90 days
Six months later, the objective finding below are essentially unchanged.
9 months following acute episode
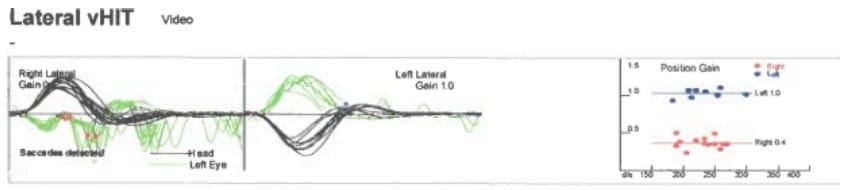
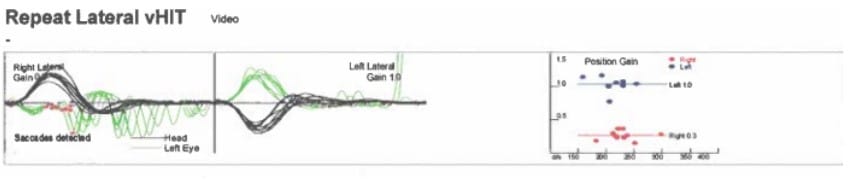
One year after the episode, I am exhibiting below mostly overt saccades with a few organized covert saccades.
One year following acute episode
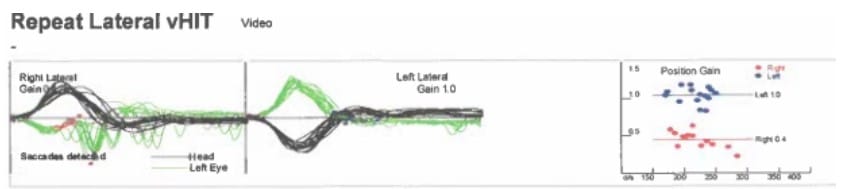
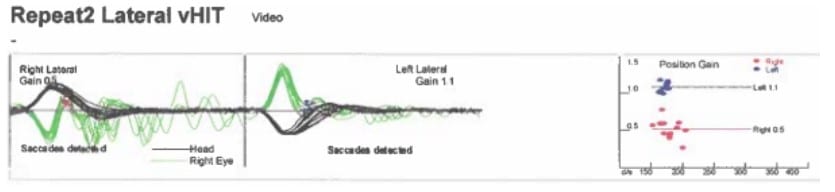
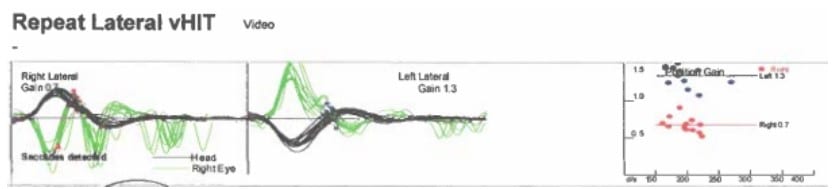
Four years after the episode, you can see below I have very organized overt saccades, with an occasional covert saccade. My colleague reported difficulty seeing any corrective saccades when performing informal head impulse test.
Four years following acute episode
Prologue
The last vHIT posted above likely represents “as good as it’s gonna get.” We have, as expected, noted that my performance on vHIT and rotational chair varies, mostly depending on how well rested I am.
I still have days where I have a low-grade spontaneous nystagmus in a vision denied (darkened) environment. I also have a strong vibration induced nystagmus every time we test.
About the Author
 Alan Desmond, AuD, is the director of the Balance Disorders Program at Wake Forest Baptist Health Center, and holds an adjunct assistant professor faculty position at the Wake Forest School of Medicine. He has written several books and book chapters on balance disorders and vestibular function. He is the co-author of the Clinical Practice Guideline for Benign Paroxysmal Positional Vertigo (BPPV). In 2015, he was the recipient of the President’s Award from the American Academy of Audiology.
Alan Desmond, AuD, is the director of the Balance Disorders Program at Wake Forest Baptist Health Center, and holds an adjunct assistant professor faculty position at the Wake Forest School of Medicine. He has written several books and book chapters on balance disorders and vestibular function. He is the co-author of the Clinical Practice Guideline for Benign Paroxysmal Positional Vertigo (BPPV). In 2015, he was the recipient of the President’s Award from the American Academy of Audiology.
*feature image shows vHIT EyeSeeCam from Interacoustics