“Peeling the Onion” is a monthly column by Harvey Abrams, PhD.
We like to think of Audiology as a doctoring profession. Those who practice the profession have the requisite training, license and letters after their names.
Amending a Barrier to Our Doctoring Vision
While we (and our patients) may view ourselves as doctors, the federal government, state governments and, by extension, most insurance companies do not recognize audiologists as practicing at the same level as medical, dental, or optometric physicians, as the services we provide and the reimbursement we receive for those services require a physician’s referral.
An initiative has been launched to modify that requirement and permit direct referral and reimbursement to audiologists through federal legislation – the Audiology Patient Choice Act of 2015 (H.R. 2519) which:
Amends title XVIII (Medicare) of the Social Security Act to revise the coverage of audiology services to treat as physicians qualified audiologists authorized by the state and acting within the scope of their licenses to furnish such services. Enables Medicare beneficiaries to choose a qualified audiologist without regard to any requirement to be under the care of (or referred by) a physician or other health care practitioner, or that services be provided under the supervision of a physician or other health care practitioner.
I wish us luck. But with that title comes solemn responsibilities not the least of which is to do no harm, or in the parlance of the day, avoid medical errors. I know this does not come as news to any of you; as a matter of fact several states require training in the avoidance of medical errors as a requirement for renewal of an audiology license. Florida, where I hold my license, is one of those states.
Medical Errors Redefined from a Patient-Centered View
A recent report from the Institute of Medicine (IOM) has brought the issue of medical errors, once again, to the forefront. Nor is this the first time IOM has addressed the problem of medical errors. In 1999 IOM issued a report called To Err is Human which offered specific repair strategies to a healthcare environment which, at that time, was costing the lives of anywhere between 44,000 to 98,000 American lives to preventable medical errors at an economic cost of between $17 billion and $29 billion (the financial consequences of medical errors on additional care, lost income and disability.
IOM’s 2015 report (the full report can be ordered from here) is a continuation of that 1999 call to action as well as another landmark 2001 report on reshaping the future of American health care for the 21st century.
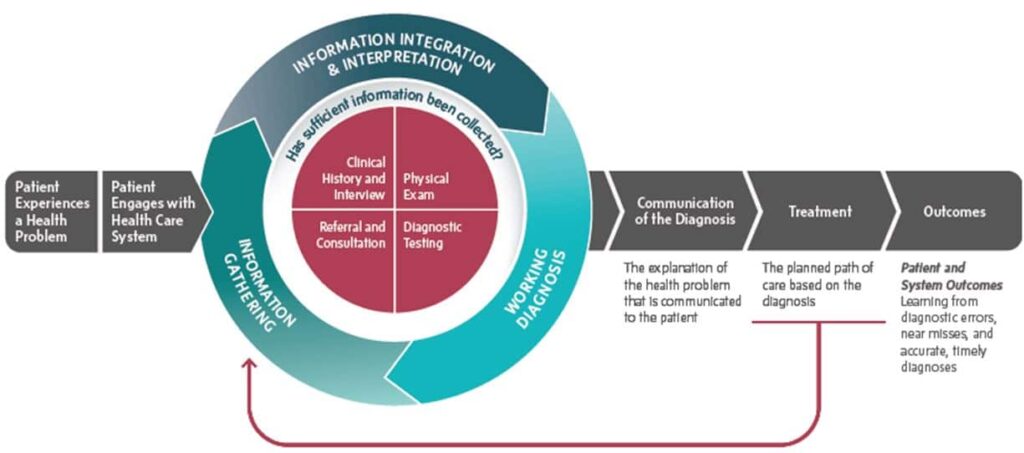
This time, IOM is focused on improving diagnosis in health care, a process that is illustrated in Figure 1. The committee that drafted the current report concluded that, “most people will experience at least one diagnostic error in their lifetime, sometimes with devastating consequences. Urgent change is warranted to address this challenge.” The committee estimates that about 5% of U.S. adults experience a diagnostic error as part of their outpatient care and that diagnostic errors contribute to 10% of patient deaths and 6% to 17% of adverse events in the hospital.
The committee defines diagnostic error as the failure to:
- establish an accurate and timely explanation of the patient’s health problem(s) or
- communicate that explanation to the patient.
This is an interesting departure from how most of us probably think of diagnostic errors which is the failure to accurately decide on the nature and circumstances of a specific disease or disorder based on the patient’s signs, symptoms, and examination results. The IOM committee’s definition takes on a more patient-centered view which, being that the patient is the victim of diagnostic errors, seems entirely appropriate and consistent with the prevailing health care trend toward patient-centered care.
Diagnostic Errors in the Audiology Doctoring Profession
How, then, should we think of the IOM report in the context of audiologic care? As noted earlier, it is our hearing and vestibular diagnostic-related services that currently define the profession in the eyes of policy makers and insurers. Importantly (and with direct applications to the audiology community), diagnostic errors, as identified in the IOM report, are not just the result of improperly interpreting examination results but can be caused by:
- inadequate collaboration and communication among clinicians, patients, and their families;
- a health care work system that is not well designed to support the diagnostic process;
- limited feedback to clinicians about diagnostic performance;
- a culture that discourages transparency and disclosure of diagnostic errors which impedes attempts to learn from these events
In reviewing your practice, do you recognize any risks for diagnostic errors reflected in the above list?
Are you communicating the explanation of your patient’s health problems in language that she understands?
Are you taking steps to mitigate those risks by improving communication and/or the culture?
Perhaps you believe that these actions are best left to others. If, however, we want the policy makers and the public to truly view us as doctors, then we, as audiologists, need to assume the responsibilities associated with a doctoring profession and become an active player in the process of reducing diagnostic errors.
This is Part 11 of the Peeling the Onion series. Click here for Part 1, Part 2, Part 3, Part 4,Part 5, Part 6, Part 7, Part 8, Part 9, Part 10.
Harvey Abrams, PhD, is a principal research audiologist in the hearing aid industry. Dr. Abrams has served in various clinical, research, and administrative capacities in the industry, the Department of Veterans Affairs and the Department of Defense. Dr. Abrams received his master’s and doctoral degrees from the University of Florida. His research has focused on treatment efficacy and improved quality of life associated with audiologic intervention. He has authored and co-authored several recent papers and book chapters and frequently lectures on post-fitting audiologic rehabilitation, outcome measures, health-related quality of life, and evidence-based audiologic practice. Dr. Abrams can be reached at [email protected]
feature image by Ross Land/Getty