Last month’s post focused on atypical causes of positional vertigo. This month’s post will be a change of pace and will consist of some general tips and tricks that we have found helpful in treating patients with BPPV.
Some of the items covered may seem rudimentary to experienced practitioners but hopefully it will be informative to others.
Correct positioning during an Epley
The head and body position must be performed correctly for an Epley maneuver or other canalith repositioning procedure (CRP) to work as designed. For clarity, the image below can be used for reference when I am describing the different positions of the Epley maneuver.
Nearly every week we see patients that have either tried home CRP or have been treated at another location and the CRP simply wasn’t performed correctly.
We predominately utilize the Epley maneuver for posterior canal BPPV and some of the common errors that we have observed include: 1: Not tilting the head backward enough in positions 2-3 to allow the otoconia to migrate around the bend in the posterior semicircular canal. 2: Lifting the head upward when going from position 2 to position 3, which causes the otoconia to reverse direction and the maneuver is less effective. 3: Not getting nose down in position 4, which prevents the otoconia from readily exiting the posterior semicircular canal.
This may seem simplistic, but it is key to get this correct for the CRP to be effective.
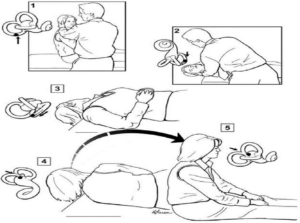
Image courtesy: https://pubmed.ncbi.nlm.nih.gov/28248609/
Home CRP for capable patients
There is disagreement among professionals as to whether we should be recommending home canalith repositioning for vestibular patients and there is a logical argument for both sides.
We personally do recommend home CRP for certain patients, only after they have been assessed clinically and they were deemed a good candidate. We also spend a considerable amount of time educating patients on the pathophysiology of BPPV and how to perform home CRP correctly. All patients that we send home with CRP either have a return visit scheduled with us or they are given the instruction to contact us if the symptoms are not resolved within a few days.
In cases of suspected BPPV with negative exam, we recommend a trial of home CRP and monitor for symptoms improvement. In cases where we know a patient has BPPV and we treat in office, there is still the chance that all the offending otoconia are not removed from the canal during the in-office repositioning. Home CRP allows for more consecutive maneuvers to clear these offending otoconia and in our experience increases the odds of quick symptom resolution.
BPPV can recur and many well-trained patients can manage symptom recurrence with home CRP.
Epley not working, then change the angle.
The effectiveness of the Epley maneuver is well known, but even the Epley doesn’t work in all cases of posterior canal BPPV. In cases where we are sure that a patient has posterior canal BPPV, but the traditional Epley maneuver is ineffective, we will often slightly change the angle in which the head is tilted backward during the maneuver.
This strategy has helped clear some stubborn cases of BPPV that were initially unresponsive. Perhaps in these cases the change in head angle helped to better mobilize any irregular shaped otoconia around the bend in the canal.
Also, there could be slight alterations in the patient’s anatomy that may make a slight modification such as this more effective for some individuals.
Vibration with cupulolithiasis
We have found skull vibration in conjunction with a CRP to be useful in cases of cupulolithiasis. In theory the vibration dislodges the adherent otoconia and allows them to be more readily repositioned.
We have found this modestly effective in cases of posterior canal cupulolithiasis as well as in cases of ageotropic horizontal canal BPPV, which some believe to be cupulolithiasis impacting the horizontal semicircular canal.
A modified Epley
In 2021 we made some modifications to the Epley maneuver for a patient with posterior canal BPPV that recently underwent arthroscopic shoulder surgery. This patient needed canalith repositioning due to posterior canal BPPV but couldn’t undergo the traditional Epley because they were unable to roll onto their shoulder for the maneuver.
We initially tried the half somersault maneuver/Foster maneuver, without any change in the symptoms. Unfortunately, we do not have access to a repositioning chair such as the Epley Omniax either. It was at that time that we created a modification to the Epley maneuver that didn’t require the patient to roll over at all. This modified maneuver was effective for this patient and has been effective on many patients since that time that were unable to undergo a traditional Epley maneuver.
I have included images below that walk through the different steps in the modification. The original case report can be found here and an update after completing the maneuver on a number of patients can be found here.
Position 1: 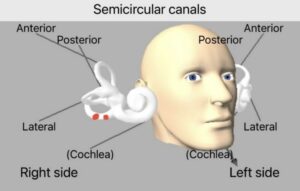
Position 2: 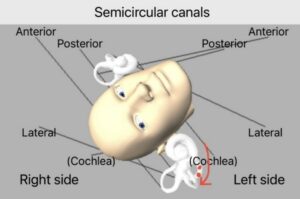
Position 3: 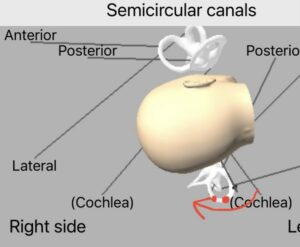
Position 4: 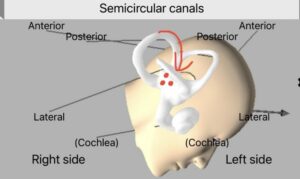
Monitoring nystagmus throughout a CRP
This only applies for clinics that have video goggles that allow you to record and monitor the eye movement. There is almost no way that you could monitor someone’s eyes throughout an entire Epley maneuver without goggles, particularly when the patient is “nose down” in position 4.
In cases of posterior canal BPPV you may observe another burst of nystagmus in either position 3 or 4 of the Epley maneuver. If you observe a transient up-beating nystagmus with a torsional component in the same direction observed during the positive Dix Hallpike, then you can be relatively sure that many of the otoconia are migrating toward the vestibule and hopefully out of the canal. You do not always observe this nystagmus, but when observed it does give some indication of the direction in which the otoconia are moving.
If in position 3 or 4 you observe a torsional component opposite to what you observed on the Dix Hallpike, then this could be otoconia reversal and likely a less effective CRP. It is important to note that this could also be observed if the individual has bilateral posterior canal BPPV as well.
For those clinics not utilizing goggles, visual fixation can be minimized with a flashlight, penlight or otoscope.
Down beating nystagmus on rising after CRP
On the completion of an Epley maneuver, in position 5, sometimes you observe a transient down beating nystagmus. This is thought to be related to otoconia debris falling out of the anterior/superior semicircular canal into the vestibule.
In many cases this is indicative that you moved the otoconia from the affected posterior semicircular canal into the vestibule and into the entrance of the anterior semicircular canal. When the person then sits upright, in position 5 of the Epley, the otoconia fall downward toward the vestibule. In our experience, this is often indicative of an effective CRP.
Loaded Dix Hallpike
We know that BPPV has a high false negative exam rate, as high as 40% in some studies. The loaded Dix Hallpike is a useful tool in cases where you expected to get a positive Dix Hallpike but did not. Essentially, you have the patient tilt their head toward their chest prior to completing a traditional Dix Hallpike.
By tilting the head forward, you allow any dislodged otoconia to settle near the cupula, then the traditional Dix Hallpike should have a greater otoconial mass to set into motion as well as a greater distance to move that mass, creating greater endolymph disturbance, and in theory generating a more obvious and prolonged nystagmus pattern.
We find this to be a useful tool and utilize it often.
Conclusions
Of course, there are exceptions for every rule and these topics only cover the high points. Hopefully these tips and tricks were helpful to some of you.







